Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Type 2 diabetes articles from across Nature Portfolio
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency of the pancreatic β-cell hormone insulin.
Advances in basic biology and translation in islet research
Advances in islet cell biology over the past few years highlight a fundamental role for intra-islet endocrine cell interactions and δ-cells in the regulation of glycaemia. New insights into how cellular heterogeneity and individual-level heterogeneity effect hormone secretion have also emerged.
- Carmella Evans-Molina

Unrestrained cancer immunity ignites atherosclerosis
Researchers map the expression of immune checkpoints and cell interactions within human atherosclerotic plaques, and the influence of relevant comorbidities such as dyslipidemia and diabetes. The findings shed light on the potential mechanisms behind the increased risk of cardiovascular events after treatment with immune checkpoint inhibitors.
- Jesse W. Williams
- Esther Lutgens
Latest Research and Reviews
Chain splitting of insulin: an underlying mechanism of insulin resistance?
- Christian N. Cramer
- František Hubálek
- Jeppe Sturis
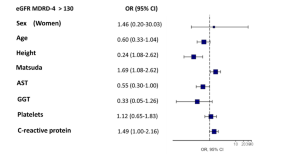
Prevalence and factors linked to renal involvement in prediabetes patients across Europe in the ePREDICE trial
- Sebastián Mas-Fontao
- Esther Civantos
- Jesús Egido
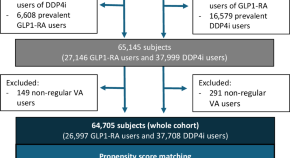
Healthcare utilization, mortality, and cardiovascular events following GLP1-RA initiation in chronic kidney disease
There is limited real-world data evaluating outcomes of glucagon-like peptide-1 receptor agonists (GLP1-RA) use in patients with moderate to advanced CKD. Here, emulating a clinical trial, the authors show that GLP1-RA use in patients with CKD is associated with lower rate of acute healthcare utilization, all-cause death and kidney events compared to DPP4i.
- Shuyao Zhang
- Ishak A. Mansi
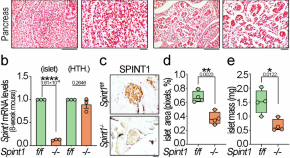
Spint1 disruption in mouse pancreas leads to glucose intolerance and impaired insulin production involving HEPSIN/MAFA
Pancreatic Spint1 disruption causes glucose intolerance, reduced islet size, and decreased insulin synthesis and secretion. SPINT1 regulates HEPSIN’s modification of GLP1R/MAFA activation, vital for glucose control by β cells, linking it to diabetes.
- Hsin-Hsien Lin
- Ming-Shyue Lee
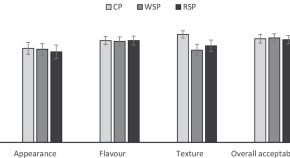
Effect of sorghum flour-containing pasta on postprandial glycemia, appetite and energy intake in healthy individuals
- Stuart K. Johnson
- Ali Madi Almajwal
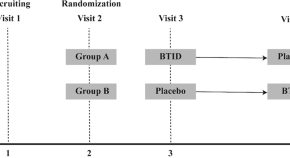
Black Tea drinks with inulin and dextrin reduced postprandial plasma glucose fluctuations in patients with type 2 diabetes: an acute, randomized, placebo-controlled, single-blind crossover study
- Danfeng Peng
News and Comment
Identification of genetic factors of type 2 diabetes mellitus risk in South Asian populations
- Olivia Tysoe
T H 1 responses in type 2 diabetes
- Stephanie Houston
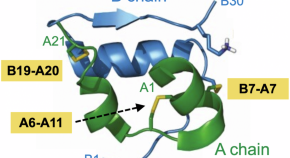
Splitting the chains: ultra-basal insulin analog uncovers a redox mechanism of hormone clearance
Reporting in Nature Communications , Kjeldsen and colleagues describe a redox mechanism of insulin clearance based on separation of A- and B chains. Exploiting an ultra-long-acting analog protected from classical clearance pathways, the study highlights principles of protein stability in pharmacology.
- Michael A. Weiss
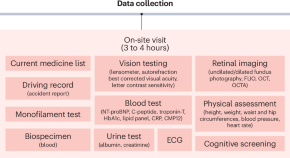
AI-READI: rethinking AI data collection, preparation and sharing in diabetes research and beyond
Here, we introduce Artificial Intelligence Ready and Equitable Atlas for Diabetes Insights (AI-READI), a multidisciplinary data-generation project designed to create and share a multimodal dataset optimized for artificial intelligence research in type 2 diabetes mellitus.
- Sally L. Baxter
- Virginia R. de Sa
- Xujing Wang
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Clinical Trials
Type 2 diabetes.
Displaying 96 studies
The purpose of this study is to identify changes to the metabolome (range of chemicals produced in the body) and microbiome (intestine microbe environment) that are unique to Roux-en-Y gastric bypass surgery and assess the associated effect on the metabolism of patients with type 2 diabetes.
The purpose of this study is to assess the impact of a whole food plant-based diet on blood sugar control in diabetic patients versus a control group on the American Diabetics Association diet before having a total hip, knee, or shoulder replacement surgery.
The purpose of this study is to learn more about if the medication, Entresto, could help the function of the heart and kidneys.
The purpose of this study is to evaluate the impact of a digital storytelling intervention derived through a community-based participatory research (CBPR) approach on type 2 diabetes mellitus (T2D) outcomes among Hispanic adults with poorly controlled type 2 diabetes mellitus (T2D) in primary care settings through a randomized clinical trial.
The primary aim of this study is to compare the outcome measures of adult ECH type 2 diabetes patients who were referred to onsite pharmacist services for management of their diabetes to similar patients who were not referred for pharmacy service management of their diabetes. A secondary aim of the study is to assess the Kasson providers’ satisfaction level and estimated pharmacy service referral frequency to their patients. A tertiary aim of the study is to compare the hospitalization rates of type 2 diabetes rates who were referred to onsite pharmacist services for management of their diabetes to similar patients ...
To explore the feasibility of conducting a family centered wellness coaching program for patients at high risk for developing diabetes, in a primary care setting.
To determine engagement patterns.
To describe characteristics of families who are likely to participate.
To identify barriers/limitations to family centered wellness coaching.
To assess whether a family centered 8 week wellness coaching intervention for primary care patients at high risk for diabetes will improve self-care behaviors as measured by self-reported changes in physical activity level and food choices.
This study is being done to understand metformin's mechanisms of action regarding glucose production, protein metabolism, and mitochondrial function.
The purpose of this study is to assess the effectiveness of Revita® DMR for improving HbA1c to ≤ 7% without the need of insulin in subjects with T2D compared to sham and to assess the effectiveness of DMR versus Sham on improvement in Glycemic, Hepatic and Cardiovascular endpoints.
The purpose of this study is to evaluate 6 weeks of home use of the Control-IQ automated insulin delivery system in individuals with type 2 diabetes.
This study will evaluate whether bile acids are able to increase insulin sensitivity and enhance glycemic control in T2DM patients, as well as exploring the mechanisms that enhance glycemic control. These observations will provide the preliminary data for proposing future therapeutic as well as further mechanistic studies of the role of bile acids in the control of glycemia in T2DM.
The purpose of this study is to determine if Inpatient Stress Hyperglycemia is an indicator of future risk of developing type 2 Diabetes Mellitus.
The GRADE Study is a pragmatic, unmasked clinical trial that will compare commonly used diabetes medications, when combined with metformin, on glycemia-lowering effectiveness and patient-centered outcomes.
The overall goal of this proposal is to determine the effects of acute hyperglycemia and its modulation by Glucagon-like Peptide-1 (GLP-1) on myocardial perfusion in type 2 diabetes (DM). This study plan utilizes myocardial contrast echocardiography (MCE) to explore a) the effects of acute hyperglycemia on myocardial perfusion and coronary flow reserve in individuals with and without DM; and b) the effects of GLP-1 on myocardial perfusion and coronary flow reserve during euglycemia and hyperglycemia in DM. The investigators will recruit individuals with and without DM matched for age, gender and degree of obesity. The investigators will measure myocardial perfusion ...
The purpose of this study is to test the hypothesis that patients with T2DM will have greater deterioration in BMSi and in cortical porosity over 3 yrs as compared to sex- and age-matched non-diabetic controls; and identify the circulating hormonal (e.g., estradiol [E2], testosterone [T]) and biochemical (e.g., bone turnover markers, AGEs) determinants of changes in these key parameters of bone quality, and evaluate the possible relationship between existing diabetic complications and skeletal deterioration over time in the T2DM patients.
The purpose of this study is to determine the effect of endogenous GLP-1 secretion on islet function in people with Typr 2 Diabetes Mellitus (T2DM).
GLP-1 is a hormone made by the body that promotes the production of insulin in response to eating. However, there is increasing evidence that this hormone might help support the body’s ability to produce insulin when diabetes develops.
The purpose of this study is to assess whether psyllium is more effective in lowering fasting blood sugar and HbA1c, and to evaluate the effect of psyllium compared to wheat dextrin on the following laboratory markers: LDL-C, inflammatory markers such as ceramides and hsCRP, and branch chain amino acids which predict Diabetes Mellitus (DM).
The purpose of this study is to assess the effectiveness of a digital storytelling intervention derived through a community based participatory research (CBPR) approach on self-management of type 2 diabetes (T2D) among Somali adults.
The purpose of this study is to find the inheritable changes in genetic makeup that are related to the development of type 2 diabetes in Latino families.
The objective of this early feasibility study is to assess the feasibility and preliminary safety of the Endogenex Divice for endoscopic duodenal mucosal regeneration in patients with type 2 diabetes (T2D) inadequately controlled on 2-3 non-insulin glucose-lowering medications.
This trial is a multi-center, adaptive, randomized, double-blind, placebo- and active- controlled, parallel group, phase 2 study in subjects with Type 2 Diabetes Mellitus to evaluate the effect of TTP399 on HbA1c following administration for 6 months.
This observational study is conducted to determine how the duodenal layer thicknesses (mucosa, submucosa, and muscularis) vary with several factors in patients with and without type 2 diabetes.
The purpose of this study is to assess penile length pre- and post-completion of RestoreX® traction therapy compared to control groups (no treatment) among men with type II diabetes.
This mixed methods study aims to answer the question: "What is the work of being a patient with type 2 diabetes mellitus?" .
The purpose of this study is to determine the impact of patient decision aids compared to usual care on measures of patient involvement in decision-making, diabetes care processes, medication adherence, glycemic and cardiovascular risk factor control, and use of resources in nonurban practices in the Midwestern United States.
The purpose of this study is to evaluate if breathing pure oxygen overnight affects insulin sensitivity in participants with diabetes.
The purpose of this study is to estimate the risk of diabetes related complications after total pancreatectomy. We will contact long term survivors after total pancreatectomy to obtain data regarding diabetes related end organ complications.
The purpose of this study is to understand nighttime glucose regulation in humans and find if the pattern is different in people with Type 2 diabetes
The study is being undertaken to understand how a gastric bypass can affect a subject's diabetes even prior to their losing significant amounts of weight. The hypothesis of this study is that increased glucagon-like peptide-1 (GLP-1) secretion explains the amelioration in insulin secretion after Roux-en-Y Gastric Bypass (RYGB) surgery.
The study purpose is to understand patients’ with the diagnosis of Diabetes Mellitus type 1 or 2 perception of the care they receive in the Diabetes clinic or Diabetes technology clinic at Mayo Clinic and to explore and to identify the healthcare system components patients consider important to be part of the comprehensive regenerative care in the clinical setting.
However, before we can implement structural changes or design interventions to promote comprehensive regenerative care in clinical practice, we first need to characterize those regenerative practices occurring today, patients expectations, perceptions and experiences about comprehensive regenerative care and determine the ...
It is unknown how patient preferences and values impact the comparative effectiveness of second-line medications for Type 2 diabetes (T2D). The purpose of this study is to elicit patient preferences toward various treatment outcomes (e.g., hospitalization, kidney disease) using a participatory ranking exercise, use these rankings to generate individually weighted composite outcomes, and estimate patient-centered treatment effects of four different second-line T2D medications that reflect the patient's value for each outcome.
The purpose of this mixed-methods study is to deploy the tenets of Health and Wellness Coaching (HWC) through a program called BeWell360 model , tailored to the needs of Healthcare Workers (HCWs) as patients living with poorly-controlled Type 2 Diabetes (T2D). The objective of this study is to pilot-test this novel, scalable, and sustainable BeWell360 model that is embedded and integrated as part of primary care for Mayo Clinic Employees within Mayo Clinic Florida who are identified as patients li)ving with poorly-controlled T2D.
The investigators will determine whether people with high muscle mitochondrial capacity produce higher amount of reactive oxygen species (ROS) on consuming high fat /high glycemic diet and thus exhibit elevated cellular oxidative damage. The investigators previously found that Asian Indian immigrants have high mitochondrial capacity in spite of severe insulin resistance. Somalians are another new immigrant population with rapidly increasing prevalence of diabetes. Both of these groups traditionally consume low caloric density diets, and the investigators hypothesize that when these groups are exposed to high-calorie Western diets, they exhibit increased oxidative stress, oxidative damage, and insulin resistance. The investigators will ...
The purpose of this research is to find out how genetic variations in GLP1R, alters insulin secretion, in the fasting state and when blood sugars levels are elevated. Results from this study may help us identify therapies to prevent or reverse type 2 diabetes mellitus.
To determine if the EndoBarrier safely and effectively improves glycemic control in obese subjects with type 2 diabetes.
The purpose of this study is to assess key characteristics of bone quality, specifically material strength and porosity, in patients who have type 2 diabetes. These patients are at an unexplained increased risk for fractures and there is an urgent need to refine clinical assessment for this risk.
Can QBSAfe be implemented in a clinical practice setting and improve quality of life, reduce treatment burden and hypoglycemia among older, complex patients with type 2 diabetes?
Questionnaire administered to diabetic patients in primary care practice (La Crosse Mayo Family Medicine Residency /Family Health Clinic) to assess patient’s diabetic knowledge. Retrospective chart review will also be done to assess objective diabetic control based on most recent hemoglobin A1c.
The objectives of this study are to identify circulating extracellular vesicle (EV)-derived protein and RNA signatures associated with Type 2 Diabetes (T2D), and to identify changes in circulating EV cargo in patients whose T2D resolves after sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB).
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for muscle insulin resistance, although it has been shown that raising FFA with Intralipid can cause muscle insulin resistance within 4 hours. We do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We propose to alter the profile and concentrations of FFA of healthy, non-obese adults using an overnight, intra-duodenal palm oil infusion vs. ...
This research study is being done to develop educational materials that will help patients and clinicians talk about diabetes treatment and management options.
The purpose of this study evaluates a subset of people with isolated Impaired Fasting Glucose with Normal Glucose Tolerance (i.e., IFG/NGT) believed to have normal β-cell function in response to a glucose challenge, suggesting that – at least in this subset of prediabetes – fasting glucose is regulated independently of glucose in the postprandial period. To some extent this is borne out by genetic association studies which have identified loci that affect fasting glucose but not glucose tolerance and vice-versa.
Assessment of glucose metabolism and liver fat after 12 week dietary intervention in pre diabetes subjects. Subjects will be randomized to either high fat (olive oil supplemented),high carb/high fiber (beans supplemented) and high carb/low fiber diets. Glucose metabolism will be assessed by labeled oral glucose tolerance test and liver fat by magnetic resonance spectroscopy pre randomization and at 8 and 12 week after starting dietary intervention.
To study the effect of an ileocolonic formulation of ox bile extract on insulin sensitivity, postprandial glycemia and incretin levels, gastric emptying, body weight and fasting serum FGF-19 (fibroblast growth factor) levels in overweight or obese type 2 diabetic subjects on therapy with DPP4 (dipeptidyl peptidase-4) inhibitors (e.g. sitagliptin) alone or in combination with metformin.
The purpose of this study is to evaluate whether or not a 6 month supply (1 meal//day) of healthy food choices readily available in the patient's home and self management training including understanding of how foods impact diabetes, improved food choices and how to prepare those foods, improve glucose control. In addition, it will evaluate whether or not there will be lasting behavior change modification after the program.
The purpose of this study is to compare the rate of progression from prediabetes at 4 months to frank diabetes at 12 months (as defined by increase in HbA1C or fasting BS to diabetic range based on the ADA criteria) after transplantation in kidney transplant recipients on Exenatide SR + SOC vs. standard-of-care alone.
The purpose of this study is to learn more about how the body stores dietary fat. Medical research has shown that fat stored in different parts of the body can affect the risk for diabetes, heart disease and other major health conditions.
The purpose of this study is to determine the mechanism(s) by which common bariatric surgical procedures alter carbohydrate metabolism. Understanding these mechanisms may ultimately lead to the development of new interventions for the prevention and treatment of type 2 diabetes and obesity.
The purpose of this study is to see why the ability of fat cells to respond to insulin is different depending on body shape and how fat tissue inflammation is involved.
This study is designed to compare an intensive lifestyle and activity coaching program ("Sessions") to usual care for diabetic patients who are sedentary. The question to be answered is whether the Sessions program improves clinical or patient centric outcomes. Recruitment is through invitiation only.
The purpose of this study is to evaluate the effects of improving glycemic control, and/or reducing glycemic variability on gastric emptying, intestinal barrier function, autonomic nerve functions, and epigenetic changes in subjects with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) who are switched to intensive insulin therapy as part of clinical practice.
A research study to enhance clinical discussion between patients and pharmacists using a shared decision making tool for type 2 diabetes or usual care.
While the potential clinical uses of pulsed electromagnetic field therapy (PEMF) are extensive, we are focusing on the potential benefits of PEMF on vascular health. We are targeting, the pre diabetic - metabolic syndrome population, a group with high prevalence in the American population. This population tends to be overweight, low fitness, high blood pressure, high triglycerides and borderline high blood glucose.
This is a study to evaluate a new Point of Care test for blood glucose monitoring.
This protocol is being conducted to determine the mechanisms responsible for insulin resistance, obesity and type 2 diabetes.
The purpose of this study is to assess the effects of a nighttime rise in cortisol on the body's glucose production in type 2 diabetes.
The goal of this study is to evaluate a new format for delivery of a culturally tailored digital storytelling intervention by incorporating a facilitated group discussion following the videos, for management of type II diabetes in Latino communities.
Integration of Diabetes Prevention Program (DPP) and Diabetes Self Management Program (DSMP) into WellConnect.
The purpose of this study is to determine the metabolic effects of Colesevelam, particularly for the ability to lower blood sugar after a meal in type 2 diabetics, in order to develop a better understanding of it's potential role in the treatment of obesity.
The purpose of this study is to test whether markers of cellular aging and the SASP are elevated in subjects with obesity and further increased in patients with obesity and Type 2 Diabetes Mellitus (T2DM) and to relate markers of cellular aging (senescence) and the SASP to skeletal parameters (DXA, HRpQCT, bone turnover markers) in each of these groups.
The goal of this study is to evaluate the presence of podocytes (special cells in the kidney that prevent protein loss) in the urine in patients with diabetes or glomerulonephritis (inflammation in the kidneys). Loss of podocyte in the urine may be an earlier sign of kidney injury (before protein loss) and the goal of this study is to evaluate the association between protein in the urine and podocytes in the urine.
The purpose of this study is to improve our understanding of why gastrointestinal symptoms occur in diabetes mellitus patients and identify new treatment(s) in the future.
These symptoms are often distressing and may impair glycemic control. We do not understand how diabetes mellitus affects the GI tracy. In 45 patients undergoing sleeve gastrectomy, we plan to compare the cellular composition of circulating peripheral mononuclear cells, stomach immune cells, and interstitial cells of Cajal in the stomach.
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM). It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking is responsible for the abnormal response to insulin. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. We will measure muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates under both saline control (high overnight FFA) and after an overnight infusion of intravenous ...
Muscle insulin resistance is a hallmark of upper body obesity (UBO) and Type 2 diabetes (T2DM), whereas lower body obesity (LBO) is characterized by near-normal insulin sensitivity. It is unknown whether muscle free fatty acid (FFA) availability or intramyocellular fatty acid trafficking differs between different obesity phenotypes. Likewise, we do not understand to what extent the incorporation of FFA into ceramides or diacylglycerols (DG) affect insulin signaling and muscle glucose uptake. By measuring muscle FFA storage into intramyocellular triglyceride, intramyocellular fatty acid trafficking, activation of the insulin signaling pathway and glucose disposal rates we will provide the first integrated examination ...
Using stem cell derived intestinal epithelial cultures (enteroids) derived from obese (BMI> 30) patients and non-obese and metabolically normal patients (either post-bariatric surgery (BS) or BS-naïve with BMI < 25), dietary glucose absorption was measured. We identified that enteroids from obese patients were characterized by glucose hyper-absorption (~ 5 fold) compared to non-obese patients. Significant upregulation of major intestinal sugar transporters, including SGLT1, GLU2 and GLUT5 was responsible for hyper-absorptive phenotype and their pharmacologic inhibition significantly decreased glucose absorption. Importantly, we observed that enteroids from post-BS non-obese patients exhibited low dietary glucose absorption, indicating that altered glucose absorption ...
The purpose of this study is to evaluate the effects of multiple dose regimens of RM-131 on vomiting episodes, stomach emptying and stomach paralysis symptoms in patients with Type 1 and Type 2 diabetes and gastroparesis.
The purpose of this study is assess the feasibility, effectiveness, and acceptability of Diabetes-REM (Rescue, Engagement, and Management), a comprehensive community paramedic (CP) program to improve diabetes self-management among adults in Southeast Minnesota (SEMN) treated for servere hypoglycemia by the Mayo Clinic Ambulance Services (MCAS).
The purpose of this study is to create a prospective cohort of subjects with increased probability of being diagnosed with pancreatic cancer and then screen this cohort for pancreatic cancer
The purpose of this study is to determine if a blood test called "pancreatic polypeptide" can help distinguish between patients with diabetes mellitus with and without pancreatic cancer.
The purpose of this study is to evaluate the effectiveness and safety of brolucizumab vs. aflibercept in the treatment of patients with visual impairment due to diabetic macular edema (DME).
Women with gestational diabetes mellitus (GDM) are likely to have insulin resistance that persists long after pregnancy, resulting in greater risk of developing type 2 diabetes mellitus (T2DM). The study will compare women with and without a previous diagnosis of GDM to determine if women with a history of GDM have abnormal fatty acid metabolism, specifically impaired adipose tissue lipolysis. The study will aim to determine whether women with a history of GDM have impaired pancreatic β-cell function. The study will determine whether women with a history of GDM have tissue specific defects in insulin action, and also identify the effect of a ...
The purpose of this study is to demonstrate feasibility of dynamic 11C-ER176 PET imaging to identify macrophage-driven immune dysregulation in gastric muscle of patients with DG. Non-invasive quantitative assessment with PET can significantly add to our diagnostic armamentarium for patients with diabetic gastroenteropathy.
Although vitreous hemorrhage (VH) from proliferative diabetic retinopathy (PDR) can cause acute and dramatic vision loss for patients with diabetes, there is no current, evidence-based clinical guidance as to what treatment method is most likely to provide the best visual outcomes once intervention is desired. Intravitreous anti-vascular endothelial growth factor (anti-VEGF) therapy alone or vitrectomy combined with intraoperative PRP each provide the opportunity to stabilize or regress retinal neovascularization. However, clinical trials are lacking to elucidate the relative time frame of visual recovery or final visual outcome in prompt vitrectomy compared with initial anti-VEGF treatment. The Diabetic Retinopathy Clinical Research ...
The purpose of this study is to assess the safety and tolerability of intra-arterially delivered mesenchymal stem/stromal cells (MSC) to a single kidney in one of two fixed doses at two time points in patients with progressive diabetic kidney disease.
Diabetic kidney disease, also known as diabetic nephropathy, is the most common cause of chronic kidney disease and end-stage kidney failure requiring dialysis or kidney transplantation. Regenerative, cell-based therapy applying MSCs holds promise to delay the progression of kidney disease in individuals with diabetes mellitus. Our clinical trial will use MSCs processed from each study participant to test the ...
This study aims to measure the percentage of time spent in hyperglycemia in patients on insulin therapy and evaluate diabetes related patient reported outcomes in kidney transplant recipients with type 2 diabetes. It also aimes to evaluate immunosuppression related patient reported outcomes in kidney transplant recipients with type 2 diabetes.
The purpose of this study is to look at how participants' daily life is affected by their heart failure. The study will also look at the change in participants' body weight. This study will compare the effect of semaglutide (a new medicine) compared to "dummy" medicine on body weight and heart failure symptoms. Participants will either get semaglutide or "dummy" medicine, which treatment participants get is decided by chance. Participants will need to take 1 injection once a week.
The purpose of this study is to evaluate whether or not semaglutide can slow down the growth and worsening of chronic kidney disease in people with type 2 diabetes. Participants will receive semaglutide (active medicine) or placebo ('dummy medicine'). This is known as participants' study medicine - which treatment participants get is decided by chance. Semaglutide is a medicine, doctors can prescribe in some countries for the treatment of type 2 diabetes. Participants will get the study medicine in a pen. Participants will use the pen to inject the medicine in a skin fold once a week. The study will close when ...
The objectives of this study are to evaluate the safety of IW-9179 in patients with diabetic gastroparesis (DGP) and the effect of treatment on the cardinal symptoms of DGP.
The purpose of this study is to evaluate the safety, tolerability, pharmacokinetics, and exploratory effectiveness of nimacimab in patients with diabetic gastroparesis.
The purpose of this study is to understand why patients with indigestion, with or without diabetes, have gastrointestinal symptoms and, in particular, to understand where the symptoms are related to increased sensitivity to nutrients.Subsequently, look at the effects of Ondansetron on these patients' symptoms.
The purpose of this study is to prospectively assemble a cohort of subjects >50 and ≤85 years of age with New-onset Diabetes (NOD):
- Estimate the probability of pancreatic ductal adenocarcinoma (PDAC) in the NOD Cohort;
- Establish a biobank of clinically annotated biospecimens including a reference set of biospecimens from pre-symptomatic PDAC and control new-onset type 2 diabetes mellitus (DM) subjects;
- Facilitate validation of emerging tests for identifying NOD subjects at high risk for having PDAC using the reference set; and
- Provide a platform for development of an interventional protocol for early detection of sporadic PDAC ...
The purpose of this study is to demonstrate the performance of the Guardian™ Sensor (3) with an advanced algorithm in subjects age 2 - 80 years, for the span of 170 hours (7 days).
The primary purpose of this study is to prospectively assess symptoms of bloating (severity, prevalence) in patients with diabetic gastroparesis.
The purpose of this study is to track the treatment burden experienced by patients living with Type 2 Diabetes Mellitus (T2DM) experience as they work to manage their illness in the context of social distancing measures.
To promote social distancing during the COVID-19 pandemic, health care institutions around the world have rapidly expanded their use of telemedicine to replace in-office appointments where possible.1 For patients with diabetes, who spend considerable time and energy engaging with various components of the health care system,2,3 this unexpected and abrupt transition to virtual health care may signal significant changes to ...
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure, disease specific biomarkers, symptoms, health status and quality of life in patients with type 2 diabetes or prediabetes and chronic heart failure with preserved systolic function.
The purpose of this study is to look at the relationship of patient-centered education, the Electronic Medical Record (patient portal) and the use of digital photography to improve the practice of routine foot care and reduce the number of foot ulcers/wounds in patients with diabetes.
Diabetes mellitus is a common condition which is defined by persistently high blood sugar levels. This is a frequent problem that is most commonly due to type 2 diabetes. However, it is now recognized that a small portion of the population with diabetes have an underlying problem with their pancreas, such as chronic pancreatitis or pancreatic cancer, as the cause of their diabetes. Currently, there is no test to identify the small number of patients who have diabetes caused by a primary problem with their pancreas.
The goal of this study is to develop a test to distinguish these ...
The purpose of this study is to evaluate the safety and efficacy of oral Pyridorin 300 mg BID in reducing the rate of progression of nephropathy due to type 2 diabetes mellitus.
The purpose of this study is to evaluate the effect of Aramchol as compared to placebo on NASH resolution, fibrosis improvement and clinical outcomes related to progression of liver disease (fibrosis stages 2-3 who are overweight or obese and have prediabetes or type 2 diabetes).
The purpose of this study is to evaluate the ability of appropriately-trained family physicians to screen for and identify Diabetic Retinopathy using retinal camera and, secondarily, to describe patients’ perception of the convenience and cost-effectiveness of retinal imaging.
The primary purpose of this study is to evaluate the impact of dapagliflozin, as compared with placebo, on heart failure disease-specific biomarkers, symptoms, health status, and quality of life in patients who have type 2 diabetes and chronic heart failure with reduced systolic function.
The purpose of this research is to determine if CGM (continuous glucose monitors) used in the hospital in patients with COVID-19 and diabetes treated with insulin will be as accurate as POC (point of care) glucose monitors. Also if found to be accurate, CGM reading data will be used together with POC glucometers to dose insulin therapy.
Hypothesis: We hypothesize that patients from the Family Medicine Department at Mayo Clinic Florida who participate in RPM will have significantly reduced emergency room visits, hospitalizations, and hospital contacts.
Aims, purpose, or objectives: In this study, we will compare the RPM group to a control group that does not receive RPM. The primary objective is to determine if there are significant group differences in emergency room visits, hospitalizations, outpatient primary care visits, outpatient specialty care visits, and hospital contacts (inbound patient portal messages and phone calls). The secondary objective is to determine if there are ...
The purpose of this study is to evaluate the effect of fenofibrate compared with placebo for prevention of diabetic retinopathy (DR) worsening or center-involved diabetic macular edema (CI-DME) with vision loss through 4 years of follow-up in participants with mild to moderately severe non-proliferative DR (NPDR) and no CI-DME at baseline.
The purpose of this study is to assess painful diabetic peripheral neuropathy after high-frequency spinal cord stimulation.
The purpose of this study is to examine the evolution of diabetic kindey injury over an extended period in a group of subjects who previously completed a clinical trial which assessed the ability of losartan to protect the kidney from injury in early diabetic kidney disease. We will also explore the relationship between diabetic kidney disease and other diabetes complications, including neuropathy and retinopathy.
The purpose of this study is to evaluate the effietiveness of remdesivir (RDV) in reducing the rate of of all-cause medically attended visits (MAVs; medical visits attended in person by the participant and a health care professional) or death in non-hospitalized participants with early stage coronavirus disease 2019 (COVID-19) and to evaluate the safety of RDV administered in an outpatient setting.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
- English (en)
- Español (es)
Recent Advances
ADA-funded researchers use the money from their awards to conduct critical diabetes research. In time, they publish their findings in order to inform fellow scientists of their results, which ensures that others will build upon their work. Ultimately, this cycle drives advances to prevent diabetes and to help people burdened by it. In 2018 alone, ADA-funded scientists published over 200 articles related to their awards!
Identification of a new player in type 1 diabetes risk
Type 1 diabetes is caused by an autoimmune attack of insulin-producing beta-cells. While genetics and the environment are known to play important roles, the underlying factors explaining why the immune system mistakenly recognize beta-cells as foreign is not known. Now, Dr. Delong has discovered a potential explanation. He found that proteins called Hybrid Insulin Peptides (HIPs) are found on beta-cells of people with type 1 diabetes and are recognized as foreign by their immune cells. Even after diabetes onset, immune cells are still present in the blood that attack these HIPs.
Next, Dr. Delong wants to determine if HIPs can serve as a biomarker or possibly even targeted to prevent or treat type 1 diabetes. Baker, R. L., Rihanek, M., Hohenstein, A. C., Nakayama, M., Michels, A., Gottlieb, P. A., Haskins, K., & Delong, T. (2019). Hybrid Insulin Peptides Are Autoantigens in Type 1 Diabetes. Diabetes , 68 (9), 1830–1840.
Understanding the biology of body-weight regulation in children
Determining the biological mechanisms regulating body-weight is important for preventing type 2 diabetes. The rise in childhood obesity has made this even more urgent. Behavioral studies have demonstrated that responses to food consumption are altered in children with obesity, but the underlying biological mechanisms are unknown. This year, Dr. Schur tested changes in brain and hormonal responses to a meal in normal-weight and obese children. Results from her study show that hormonal responses in obese children are normal following a meal, but responses within the brain are reduced. The lack of response within the brain may predispose them to overconsumption of food or difficulty with weight-loss.
With this information at hand, Dr. Schur wants to investigate how this information can be used to treat obesity in children and reduce diabetes.
Roth, C. L., Melhorn, S. J., Elfers, C. T., Scholz, K., De Leon, M. R. B., Rowland, M., Kearns, S., Aylward, E., Grabowski, T. J., Saelens, B. E., & Schur, E. A. (2019). Central Nervous System and Peripheral Hormone Responses to a Meal in Children. The Journal of Clinical Endocrinology and Metabolism , 104 (5), 1471–1483.
A novel molecule to improve continuous glucose monitoring
To create a fully automated artificial pancreas, it is critical to be able to quantify blood glucose in an accurate and stable manner. Current ways of continuously monitoring glucose are dependent on the activity of an enzyme which can change over time, meaning the potential for inaccurate readings and need for frequent replacement or calibration. Dr. Wang has developed a novel molecule that uses a different, non-enzymatic approach to continuously monitor glucose levels in the blood. This new molecule is stable over long periods of time and can be easily integrated into miniaturized systems.
Now, Dr. Wang is in the process of patenting his invention and intends to continue research on this new molecule so that it can eventually benefit people living with diabetes.
Wang, B. , Chou, K.-H., Queenan, B. N., Pennathur, S., & Bazan, G. C. (2019). Molecular Design of a New Diboronic Acid for the Electrohydrodynamic Monitoring of Glucose. Angewandte Chemie (International Ed. in English) , 58 (31), 10612–10615.
Addressing the legacy effect of diabetes
Several large clinical trials have demonstrated the importance of tight glucose control for reducing diabetes complications. However, few studies to date have tested this in the real-world, outside of a controlled clinical setting. In a study published this year, Dr. Laiteerapong found that indeed in a real-world setting, people with lower hemoglobin A1C levels after diagnosis had significantly lower vascular complications later on, a phenomenon known as the ‘legacy effect’ of glucose control. Her research noted the importance of early intervention for the best outcomes, as those with the low A1C levels just one-year after diagnosis had significantly lower vascular disease risk compared to people with higher A1C levels.
With these findings in hand, physicians and policymakers will have more material to debate and determine the best course of action for improving outcomes in people newly diagnosed with diabetes.
Laiteerapong, N. , Ham, S. A., Gao, Y., Moffet, H. H., Liu, J. Y., Huang, E. S., & Karter, A. J. (2019). The Legacy Effect in Type 2 Diabetes: Impact of Early Glycemic Control on Future Complications (The Diabetes & Aging Study). Diabetes Care , 42 (3), 416–426.
A new way to prevent immune cells from attacking insulin-producing beta-cells
Replacing insulin-producing beta-cells that have been lost in people with type 1 diabetes is a promising strategy to restore control of glucose levels. However, because the autoimmune disease is a continuous process, replacing beta-cells results in another immune attack if immunosorbent drugs are not used, which carry significant side-effects. This year, Dr. Song reported on the potential of an immunotherapy he developed that prevents immune cells from attacking beta-cells and reduces inflammatory processes. This immunotherapy offers several potential benefits, including eliminating the need for immunosuppression, long-lasting effects, and the ability to customize the treatment to each patient.
The ability to suppress autoimmunity has implications for both prevention of type 1 diabetes and improving success rates of islet transplantation.
Haque, M., Lei, F., Xiong, X., Das, J. K., Ren, X., Fang, D., Salek-Ardakani, S., Yang, J.-M., & Song, J . (2019). Stem cell-derived tissue-associated regulatory T cells suppress the activity of pathogenic cells in autoimmune diabetes. JCI Insight , 4 (7).
A new target to improve insulin sensitivity
The hormone insulin normally acts like a ‘key’, traveling through the blood and opening the cellular ‘lock’ to enable the entry of glucose into muscle and fat cells. However, in people with type 2 diabetes, the lock on the cellular door has, in effect, been changed, meaning insulin isn’t as effective. This phenomenon is called insulin resistance. Scientists have long sought to understand what causes insulin resistance and develop therapies to enable insulin to work correctly again. This year, Dr. Summers determined an essential role for a molecule called ceramides as a driver of insulin resistance in mice. He also presented a new therapeutic strategy for lowering ceramides and reversing insulin resistance. His findings were published in one of the most prestigious scientific journals, Science .
Soon, Dr. Summers and his team will attempt to validate these findings in humans, with the ultimate goal of developing a new medication to help improve outcomes in people with diabetes.
Chaurasia, B., Tippetts, T. S., Mayoral Monibas, R., Liu, J., Li, Y., Wang, L., Wilkerson, J. L., Sweeney, C. R., Pereira, R. F., Sumida, D. H., Maschek, J. A., Cox, J. E., Kaddai, V., Lancaster, G. I., Siddique, M. M., Poss, A., Pearson, M., Satapati, S., Zhou, H., … Summers, S. A. (2019). Targeting a ceramide double bond improves insulin resistance and hepatic steatosis. Science (New York, N.Y.) , 365 (6451), 386–392.

Determining the role of BPA in type 2 diabetes risk
Many synthetic chemicals have infiltrated our food system during the period in which rates of diabetes has surged. Data has suggested that one particular synthetic chemical, bisphenol A (BPA), may be associated with increased risk for developing type 2 diabetes. However, no study to date has determined whether consumption of BPA alters the progression to type 2 diabetes in humans. Results reported this year by Dr. Hagobian demonstrated that indeed when BPA is administered to humans in a controlled manner, there is an immediate, direct effect on glucose and insulin levels.
Now, Dr. Hagobian wants to conduct a larger clinical trial including exposure to BPA over a longer period of time to determine precisely how BPA influences glucose and insulin. Such results are important to ensure the removal of chemicals contributing to chronic diseases, including diabetes.
Hagobian, T. A. , Bird, A., Stanelle, S., Williams, D., Schaffner, A., & Phelan, S. (2019). Pilot Study on the Effect of Orally Administered Bisphenol A on Glucose and Insulin Response in Nonobese Adults. Journal of the Endocrine Society , 3 (3), 643–654.
Investigating the loss of postmenopausal protection from cardiovascular disease in women with type 1 diabetes
On average, women have a lower risk of developing heart disease compared to men. However, research has shown that this protection is lost in women with type 1 diabetes. The process of menopause increases rates of heart disease in women, but it is not known how menopause affects women with type 1 diabetes in regard to risk for developing heart disease. In a study published this year, Dr. Snell-Bergeon found that menopause increased risk markers for heart disease in women with type 1 diabetes more than women without diabetes.
Research has led to improved treatments and significant gains in life expectancy for people with diabetes and, as a result, many more women are reaching the age of menopause. Future research is needed to address prevention and treatment options.
Keshawarz, A., Pyle, L., Alman, A., Sassano, C., Westfeldt, E., Sippl, R., & Snell-Bergeon, J. (2019). Type 1 Diabetes Accelerates Progression of Coronary Artery Calcium Over the Menopausal Transition: The CACTI Study. Diabetes Care , 42 (12), 2315–2321.
Identification of a potential therapy for diabetic neuropathy related to type 1 and type 2 diabetes
Diabetic neuropathy is a type of nerve damage that is one of the most common complications affecting people with diabetes. For some, neuropathy can be mild, but for others, it can be painful and debilitating. Additionally, neuropathy can affect the spinal cord and the brain. Effective clinical treatments for neuropathy are currently lacking. Recently, Dr. Calcutt reported results of a new potential therapy that could bring hope to the millions of people living with diabetic neuropathy. His study found that a molecule currently in clinical trials for the treatment of depression may be valuable for diabetic neuropathy, particularly the type affecting the brain.
Because the molecule is already in clinical trials, there is the potential that it can benefit patients sooner than later.
Jolivalt, C. G., Marquez, A., Quach, D., Navarro Diaz, M. C., Anaya, C., Kifle, B., Muttalib, N., Sanchez, G., Guernsey, L., Hefferan, M., Smith, D. R., Fernyhough, P., Johe, K., & Calcutt, N. A. (2019). Amelioration of Both Central and Peripheral Neuropathy in Mouse Models of Type 1 and Type 2 Diabetes by the Neurogenic Molecule NSI-189. Diabetes , 68 (11), 2143–2154.
ADA-funded researcher studying link between ageing and type 2 diabetes
One of the most important risk factors for developing type 2 diabetes is age. As a person gets older, their risk for developing type 2 diabetes increases. Scientists want to better understand the relationship between ageing and diabetes in order to determine out how to best prevent and treat type 2 diabetes. ADA-funded researcher Rafael Arrojo e Drigo, PhD, from the Salk Institute for Biological Studies, is one of those scientists working hard to solve this puzzle.
Recently, Dr. Arrojo e Drigo published results from his research in the journal Cell Metabolism . The goal of this specific study was to use high-powered microscopes and novel cellular imaging tools to determine the ‘age’ of different cells that reside in organs that control glucose levels, including the brain, liver and pancreas. He found that, in mice, the cells that make insulin in the pancreas – called beta-cells – were a mosaic of both old and young cells. Some beta-cells appeared to be as old as the animal itself, and some were determined to be much younger, indicating they recently underwent cell division.
Insufficient insulin production by beta-cells is known to be a cause of type 2 diabetes. One reason for this is thought to be fewer numbers of functional beta-cells. Dr. Arrojo e Drigo believes that people with or at risk for diabetes may have fewer ‘young’ beta-cells, which are likely to function better than old ones. Alternatively, if we can figure out how to induce the production of younger, high-functioning beta-cells in the pancreas, it could be a potential treatment for people with diabetes.
In the near future, Dr. Arrojo e Drigo’s wants to figure out how to apply this research to humans. “The next step is to look for molecular or morphological features that would allow us to distinguish a young cell from and old cell,” Dr. Arrojo e Drigo said.
The results from this research are expected to provide a unique insight into the life-cycle of beta-cells and pave the way to novel therapeutic avenues for type 2 diabetes.
Watch a video of Dr. Arrojo e Drigo explaining his research!
Arrojo E Drigo, R. , Lev-Ram, V., Tyagi, S., Ramachandra, R., Deerinck, T., Bushong, E., … Hetzer, M. W. (2019). Age Mosaicism across Multiple Scales in Adult Tissues. Cell Metabolism , 30 (2), 343-351.e3.
Researcher identifies potential underlying cause of type 1 diabetes
Type 1 diabetes occurs when the immune system mistakenly recognizes insulin-producing beta-cells as foreign and attacks them. The result is insulin deficiency due to the destruction of the beta-cells. Thankfully, this previously life-threatening condition can be managed through glucose monitoring and insulin administration. Still, therapies designed to address the underlying immunological cause of type 1 diabetes remain unavailable.
Conventional approaches have focused on suppressing the immune system, which has serious side effects and has been mostly unsuccessful. The American Diabetes Association recently awarded a grant to Dr. Kenneth Brayman, who proposed to take a different approach. What if instead of suppressing the whole immune system, we boost regulatory aspects that already exist in the system, thereby reigning in inappropriate immune cell activation and preventing beta-cell destruction? His idea focused on a molecule called immunoglobulin M (IgM), which is responsible for limiting inflammation and regulating immune cell development.
In a paper published in the journal Diabetes , Dr. Brayman and a team of researchers reported exciting findings related to this approach. They found that supplementing IgM obtained from healthy mice into mice with type 1 diabetes selectively reduced the amount of autoreactive immune cells known to target beta-cells for destruction. Amazingly, this resulted in reversal of new-onset diabetes. Importantly, the authors of the study determined this therapy is translatable to humans. IgM isolated from healthy human donors also prevented the development of type 1 diabetes in a humanized mouse model of type 1 diabetes.
The scientists tweaked the original experiment by isolating IgM from mice prone to developing type 1 diabetes, but before it actually occurred. When mice with newly onset diabetes were supplemented with this IgM, their diabetes was not reversed. This finding suggests that in type 1 diabetes, IgM loses its capacity to serve as a regulator of immune cells, which may be contribute to the underlying cause of the disease.
Future studies will determine exactly how IgM changes its regulatory properties to enable diabetes development. Identification of the most biologically optimal IgM will facilitate transition to clinical applications of IgM as a potential therapeutic for people with type 1 diabetes. Wilson, C. S., Chhabra, P., Marshall, A. F., Morr, C. V., Stocks, B. T., Hoopes, E. M., Bonami, R.H., Poffenberger, G., Brayman, K.L. , Moore, D. J. (2018). Healthy Donor Polyclonal IgM’s Diminish B Lymphocyte Autoreactivity, Enhance Treg Generation, and Reverse T1D in NOD Mice. Diabetes .
ADA-funded researcher designs community program to help all people tackle diabetes
Diabetes self-management and support programs are important adjuncts to traditional physician directed treatment. These community-based programs aim to give people with diabetes the knowledge and skills necessary to effectively self-manage their condition. While several clinical trials have demonstrated the value of diabetes self-management programs in terms of improving glucose control and reducing health-care costs, whether this also occurs in implemented programs outside a controlled setting is unclear, particularly in socially and economically disadvantaged groups.
Lack of infrastructure and manpower are often cited as barriers to implementation of these programs in socioeconomically disadvantaged communities. ADA-funded researcher Dr. Briana Mezuk addressed this challenge in a study recently published in The Diabetes Educator . Dr. Mezuk partnered with the YMCA to evaluate the impact of the Diabetes Control Program in Richmond, Virginia. This community-academic partnership enabled both implementation and evaluation of the Diabetes Control Program in socially disadvantaged communities, who are at higher risk for developing diabetes and the complications that accompany it.
Dr. Mezuk had two primary research questions: (1) What is the geographic and demographic reach of the program? and (2) Is the program effective at improving diabetes management and health outcomes in participants? Over a 12-week study period, Dr. Mezuk found that there was broad geographic and demographic participation in the program. The program had participants from urban, suburban and rural areas, most of which came from lower-income zip codes. HbA1C, mental health and self-management behaviors all improved in people taking part in the Greater Richmond Diabetes Control Program. Results from this study demonstrate the value of diabetes self-management programs and their potential to broadly improve health outcomes in socioeconomically diverse communities. Potential exists for community-based programs to address the widespread issue of outcome disparities related to diabetes. Mezuk, B. , Thornton, W., Sealy-Jefferson, S., Montgomery, J., Smith, J., Lexima, E., … Concha, J. B. (2018). Successfully Managing Diabetes in a Community Setting: Evidence from the YMCA of Greater Richmond Diabetes Control Program. The Diabetes Educator , 44 (4), 383–394.
Using incentives to stimulate behavior changes in youth at risk for developing diabetes
Once referred to as ‘adult-onset diabetes’, incidence of type 2 diabetes is now rapidly increasing in America’s youth. Unfortunately, children often do not have the ability to understand how everyday choices impact their health. Could there be a way to change a child’s eating behaviors? Davene Wright, PhD, of Seattle Children’s Hospital was granted an Innovative Clinical or Translational Science award to determine whether using incentives, directed by parents, can improve behaviors related to diabetes risk. A study published this year in Preventive Medicine Reports outlined what incentives were most desirable and feasible to implement. A key finding was that incentives should be tied to behavior changes and not to changes in body-weight.
With this information in hand, Dr. Wright now wants to see if incentives do indeed change a child’s eating habits and risk for developing type 2 diabetes. She is also planning to test whether an incentive program can improve behavior related to diabetes management in youth with type 1 diabetes. Jacob-Files, E., Powell, J., & Wright, D. R. (2018). Exploring parent attitudes around using incentives to promote engagement in family-based weight management programs. Preventive Medicine Reports , 10 , 278–284.
Determining the genetic risk for gestational diabetes
Research has identified more than 100 genetic variants linked to risk for developing type 2 diabetes in humans. However, the extent to which these same genetic variants might affect a woman’s probability for getting gestational diabetes has not been investigated.
Pathway to Stop Diabetes ® Accelerator awardee Marie-France Hivert, MD, of Harvard University set out to answer this critical question. Dr. Hivert found that indeed genetic determinants of type 2 diabetes outside of pregnancy are also strong risk factors for gestational diabetes. This study was published in the journal Diabetes .
The implications? Because of this finding, doctors in the clinic may soon be able to identify women at risk for getting gestational diabetes and take proactive steps to prevent it. Powe, C. E., Nodzenski, M., Talbot, O., Allard, C., Briggs, C., Leya, M. V., … Hivert, M.-F. (2018). Genetic Determinants of Glycemic Traits and the Risk of Gestational Diabetes Mellitus. Diabetes , 67 (12), 2703–2709.

Give Today and Change lives!
With your support, the American Diabetes Association® can continue our lifesaving work to make breakthroughs in research and provide people with the resources they need to fight diabetes.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Association of risk factors with type 2 diabetes: A systematic review
Leila ismail, huned materwala, juma al kaabi.
- Author information
- Article notes
- Copyright and License information
Corresponding author. [email protected]
Received 2020 Nov 5; Revised 2021 Feb 28; Accepted 2021 Mar 1; Collection date 2021.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Diabetes is the leading cause of severe health complications and one of the top 10 causes of death worldwide. To date, diabetes has no cure, and therefore, it is necessary to take precautionary measures to avoid its occurrence. The main aim of this systematic review is to identify the majority of the risk factors for the incidence/prevalence of type 2 diabetes mellitus on one hand, and to give a critical analysis of the cohort/cross-sectional studies which examine the impact of the association of risk factors on diabetes. Consequently, we provide insights on risk factors whose interactions are major players in developing diabetes. We conclude with recommendations to allied health professionals, individuals and government institutions to support better diagnosis and prognosis of the disease.
Keywords: Aging, Cardiovascular disease, Depression, Diabetes mellitus, Dyslipidemia, Ethnicity, Family history of diabetes, Hypertension, Physical inactivity, Prevention, Risk factors, Serum uric acid, Sleep quality, Sleep quantity, Smoking, Type 2 diabetes, Obesity
1. Introduction
Diabetes Mellitus (DM) commonly referred to as diabetes, is a chronic disease that affects how the body turns food into energy [1] . It is one of the top 10 causes of death worldwide causing 4 million deaths in 2017 [2] , [3] . According to a report by the International Diabetes Federation (IDF) [3] , the total number of adults (20–79 years) with diabetes in 2045 will be 629 million from 425 million in 2017 (48% increase). In 2017, diabetes caused at least 727 billion USD in health expenditure, which is 12% of the total spending on adults [3] . According to the National Diabetes Statistics Report [4] , 30.3 million (9.4% of the US population) people have diabetes, and 84.1 million (29.06% of the population) have pre-diabetes. 1 in 2 people (212 million) with diabetes was undiagnosed in 2017 according to IDF [5] . Diabetes if left untreated can cause serious medical issues, such as cardiovascular disease, stroke, chronic kidney disease, foot ulcers, damage to the eyes, and prolonged kidney ailment. To date, there is no permanent cure for diabetes and the patients have to rely on healthy lifestyle and timely medication [6] .
There are three main types of diabetes: type 1, type 2, and gestational diabetes (diabetes while pregnant) [1] . Type 1 diabetes mostly occurs in children and adolescents. 1,106,500 children were suffering from type 1 diabetes in 2017 [3] . The symptoms of type 1 diabetes include abnormal thirst and dry mouth, frequent urination, fatigue, constant hunger, sudden weight loss, bed-wetting, and blurred vision. Type 2 diabetes is mostly seen in adults, but it is increasing in children and adolescents due to the rising level of obesity, physical inactivity and unhealthy diet [5] . 372 million adults were at the risk of developing type 2 diabetes in 2019 [3] . In 2017, more than 21 million live births were affected by diabetes during pregnancy [3] . In this paper, we focus on type 2 diabetes due to the alarming numbers.
Type 2 Diabetes is thought to prevail in an individual from an interaction between several lifestyle, medical condition, hereditary, psychosocial and demographic risk factors such as high-level serum uric acid, sleep quality/quantity, smoking, depression, cardiovascular disease, dyslipidemia, hypertension, aging, ethnicity, family history of diabetes, physical inactivity, and obesity [6] . In this paper, we present a systematic review of the literature on the association of these risk factors with the incidence/prevalence of type 2 diabetes. We give insights on the contribution of independent risk factors in the development of type 2 diabetes along with possible solutions towards a preventive approach.
We conduct a systematic literature search using CINAHL, IEEE Xplore, Embase, MEDLINE, PubMed Central, ScienceDirect, Scopus, Springer, and Web of Science databases. Our search criteria does not include a time bound. Its main objective is to retrieve all the studies which examine the association between individual risk factors and the incidence/prevalence of type 2 diabetes. Table A1 shows the search string used for each risk factor. The relevant studies have to meet the following inclusion criteria: 1) published in the English language, 2) prospective cohort or cross-sectional study, 3) type 2 diabetes as a specified risk, 4) one of its risk factors, 5) findings in terms of Odds Ratio (OR), Risk Ratio/Relative Risk (RR), or Hazard Ratio (HR), and the corresponding 95% Confidence Intervals (CIs) for the association between the risk factor and type 2 diabetes. To assess the quality of the studies, we use the National Institutes of Health (NIH) quality assessment tool [7] . The tool consists of 14 questions to evaluate the validity and bias risk of a study. We answered each question by either yes, no, cannot be determined, not applicable, or not reported. The tool then classifies each study as high quality (Good), moderate quality (Fair) and low quality (Poor).
Fig. 1 shows the result of our systematic approach that is used to screen the relevant studies. Irrelevant studies that do not meet the inclusion criteria mentioned in the previous section were excluded after screening titles, abstracts and full texts. At last, 106 papers are considered for this review. These papers are divided into ten categories based on the risk factor under study ( Fig. 1 ). Our review reveals that there is no study that examines the association of age or physical inactivity as an independent risk factor with type 2 diabetes. Table A2 shows the quality assessment results for the studies included in this paper. For smoking, cardiovascular disease and hypertension risk factors, the majority of the studies are of high quality. For serum uric acid, sleep quantity/quality, depression, dyslipidemia, ethnicity, family history of diabetes and obesity, the majority of the studies are of moderate quality.
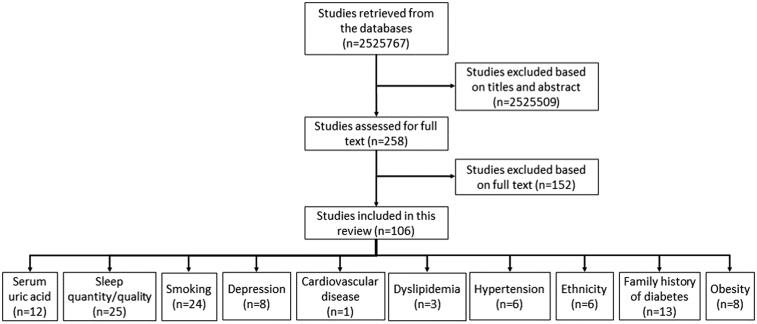
Flowchart of the selection of relevant studies.
3.1. Serum uric acid
Serum uric acid, a common component of urine generated by the metabolic breakdown of purines, have been associated with insulin resistance and type 2 diabetes [8] . High serum uric acid level in an individual leads to: 1) nitric-oxide mediated vasoconstriction (contraction of blood vessels) leading to impaired glucose uptake in the muscles [9] , 2) increase in oxidative stress [10] and 3) increase in inflammation leading to a decrease in adiponectin [11] , [12] . Consequently, the blood glucose level increases leading to dysfunctional and eventually dead beta-cells [13] . As a result, the individual develops type 2 diabetes. Table 1 shows the characteristics and findings of the work in the literature studying the association between high serum uric acid level and type 2 diabetes.
Characteristics and findings of the studies examining the association between high level serum uric acid and type 2 diabetes.
RS-Random Sample, MONICA-Multinational MONItoring of trends and determinants in CArdiovascular disease, ARIC-Atherosclerosis Risk in Communities, FDPS-Finnish Diabetes Prevention Study, CSCCS-Chin Shan Community Cardiovascular study, MRFIT-Multiple Risk Factor Intervention Trial, NHANES-National Health and Nutrition Examination Survey, QFS-Quebec Family Study, M-Men, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
Perry et al. [14] found that an individual having a uric acid level of more than 411 μ mol/l is at 1.5 times more risk of developing type 2 diabetes compared to an individual having uric acid level less than 302 μ mol/l. Niskanen et al. [15] also confirmed that change in uric acid levels is associated with a 2 times increase in the risk of incidence type 2 diabetes. Dehghan et al. [16] in their study showed that individuals having uric acid level > 370 μ mol/l are at high risk of incidence type 2 diabetes (HR 1.68, 95% CI 1.22–2.30) compared to those having uric acid level ⩽ 267 μ mol/l. The authors concluded that lowering uric acid level can be a novel approach for diabetes prevention. Xu et al. [17] found that the association between high serum uric acid level and diabetes is the same in both men and women (RR 1.131, 95% CI 1.084–1.179). The association (RR 1.17, 95% CI 1.09–1.25) is also examined by Kodama et al. [18] . Nakagawa et al. [19] showed that uric acid is a significant and independent risk factor in predicting hyperinsulinemia. The authors observed that serum uric acid level ⩾ 5.5 mg/dl is associated with the development of hyperinsulinemia after 6 months (OR 5.47, 90% CI 1.6–1.77) and 12 months (OR 3.4, 90% CI 1.1–10.4). However, the cohort was controlled for gender and age ( > 60 years). Consequently, it can not be concluded whether uric acid is an independent risk factor or there is an integrated effect of uric acid, gender and age.
Several studies argue that high-level uric acid is not an independent risk factor and it only emphasizes the association between independent risk factors such as age, obesity, hypertension, gender, and dyslipidemia, and type 2 diabetes [20] . Chou et al. show that uric acid has a significant association with type 2 diabetes in old and obese individuals [21] . Another study by Meisinger et al. [22] shows that high-level uric acid is associated with incidence of type 2 diabetes in women only with HR 2.5 per 1 mmol/L increase. Carnethon et al. [23] found that the risk of incidence type 2 diabetes increases (OR 1.3, (1.2–1.4)) with every 1.4 mg/dl increase in uric acid level. However, this is in combination with an increase in waist/hip ratio, smoking and obesity. Chien et al. [24] stated that individuals with a uric acid level of 0.486 mmol/L and having metabolic syndrome have a 3.3 times more risk of incidence type 2 diabetes compared to those with a uric acid level of 0.211 mmol/L and not having metabolic syndrome. Nan et al. [25] examined the impact of ethnicity and gender on the association between uric acid and incidence of type 2 diabetes. The authors found that the high serum uric acid is an independent risk factor for type 2 diabetes in Mauritian Indian men compared to Creole men, and there is a no-to-weak association in women of both ethnicity. Similarly, Choi et al. [26] studied the association between uric acid and type 2 diabetes in men having cardiovascular risk profile. The authors concluded that men with cardiovascular profile having high uric acid level are twice likely to develop type 2 diabetes. The authors also stated that this association between uric acid and diabetes is independent of other risk factors such as obesity, age, family history of diabetes, hypertension, and metabolic syndrome. Kramer et al. [27] analyzed the impact of age and impaired fasting glucose (IFG) on the association and found that high uric acid level can independently predict incidence of type 2 diabetes (OR 1.65, 95% CI 1.25–2.18) in older adults having IFG. Lv et al. [28] found that high serum uric acid level is associated to type 2 diabetes in middle-aged or older people (RR 1.56, 95% CI 1.39–1-76).
In summary, the association between high-level serum uric acid remains obscure. It is debatable whether serum uric acid is an independent risk factor for type 2 diabetes or it only emphasizes the association between other independent risk factors and type 2 diabetes. Some studies reported a positive association between high serum uric acid level and incidence of type 2 diabetes [14] , [15] , [16] , [19] , [24] , whereas others [25] , [29] reported no association. On the contrary, some studies reported an inverse association between uric acid and diabetes [30] , [31] , [32] . Furthermore, some studies argue that there is a reverse association, i.e., diabetes leads to high uric acid levels [33] , [34] .
3.2. Sleep quantity/quality
The quality and quantity of sleep are affected by several cultural, social, behavioral, psychological, and environmental factors. The working professionals often experience fatigue, tiredness and daytime napping due to irregular working hours and shifts. Evidence shows that the current average sleep of an individual, i.e., 6.8 h/night, is 1.5 h less than that a century ago [45] . The cause of sleep loss is multi-factorial. For instance 45% of adults report that they sleep fewer hours to get more work done, 43% reported that they watch television or use the Internet, and 22% reported to be suffering from insomnia. The unusual, disturbed and reduced sleep is associated with glucose intolerance [46] .
An individual suffering from sleep disorder, known as obstructive sleep apnea (OSA), experiences: 1) deficiency in the amount of oxygen reaching the tissues by total/partial collapse of upper airways while sleeping (hypoxia) and 2) inflammation. Frequent Hypoxia triggers an increase in sympathetic activity [47] . Increased sympathetic activity and inflammation lead to insulin resistance condition [48] , [49] and eventually to type 2 diabetes. Table 2 shows the characteristics and findings of the work in the literature studying the association between sleep quantity/quality and type 2 diabetes.
Characteristics and findings of the studies examining the association between sleep quantity/quality and type 2 diabetes.
DIS-Difficulty Initiating Sleep, DMS-Difficulty Maintaining Sleep, EPIC-European Prospective Investigation into Cancer and Nutrition, FIN D2D-Finnish type 2 Diabetes, HIPOP-OHP-High risk and Population Strategy for Occupational Health Promotion, IHHP-Isfahan Healthy Heart Program, IRAS-Insulin Resistance Atherosclerosis Study, M-Men, MC-Millennium Cohort, MMAS-Massachusetts Male Aging Study, MONICA-Multinational MONItoring of trends and determinants in CArdiovascular disease, MPP-Malmo Preventive Project, NHANES-National Health and Nutrition Examination Survey, NHIS-National Health Interview Survey, NHS-Nurse Health Study, NHW-Non Hispanic Whites, NIH AARP-National Institutes of Health American Association of Retired Persons Diet and Health Study, QFS-Quebec Family Study, RS-Random Sample, SHHS-Sleep Heart Health Study, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
The results in the literature show that compared to a reference sleep duration of 7-8 h, an individual having either short sleep duration ( < 6 h) or long sleep duration ( > 8 h) is at high risk of developing type 2 diabetes. However, [50] , [51] concluded that there is no significant association between sleep and incidence of type 2 diabetes. Mallon et al. [52] studied the impact of gender on the association between sleep and diabetes. The authors concluded that short sleep duration increases the risk of incidence diabetes in men, whereas, in women, long sleep duration dominates. The effect of ethnicity on the association is analyzed by [53] , [54] , [55] . Zizi et al. [53] and Jackson et al. [54] showed that the prevalence of type 2 diabetes is more in whites who sleep less than 5 h or more than 8 -9 h compared to blacks. Beihl [55] showed that the association is more in Hispanics/Non-Hispanic Whites compared to that in African-American. Xu et al. examined the association between day-time napping and type 2 diabetes and showed that an individual taking more than 1 h of day-time nap is at 1.5 times more risk to develop diabetes compared to an individual who does not take a nap during the day. In the context of sleep quality, the risk of incidence type 2 diabetes is more in an individual having difficulty initiating sleep (DIS), and the risk increases with increasing DIS frequency [56] , [57] , [58] . Furthermore, the association is more in women having DIS compared to men [59] .
In summary, there is a strong association between sleep quantity/quality and the incidence of type 2 diabetes. The association is stronger in women sleeping for more duration and in men with short sleep duration. Moreover, this association is affected by ethnicity.
3.3. Smoking
Smoking leads to more than 8 million deaths per year [60] . This is from both active and passive uses, i.e, non-smokers exposed to smokers. Smokers are 30–40% more likely to develop type 2 diabetes compared to non-smokers [61] . When an individual smokes, the level of nicotine increases in his/her body. This leads to a reduction in muscle glucose intake, developing insulin resistance and leading to type 2 diabetes [62] . The characteristics and findings of table:smokingtable:smoking/passive smoking and the incidence of type 2 diabetes are presented in Table 3 .
Characteristics and findings of the studies examining the association between smoking and type 2 diabetes.
ZS-Zutphen Study, NHS-Nurse Health Study, NHIS-National Health Interview Survey, HPFS-Health Professionals’ Follow-up Study, RS-Random Sample, SOF-Study of Osteoporotic Fractures, OHS-Osaka Health Survey, PHS-Physicians Health Survey, BRHS-British Regional Health Study, CPS-Cancer Prevention Study, NCDS-National Child Development Study, RIH-Regional Institute for Health, NTHS-Nord Trondelag Health Survey, IRAS-Insulin Resistance Atherosclerosis Study, ARIC-Atherosclerosis Risk in Communities, KCPS-Korean Cancer Prevention Study, JPHC-Japan Public Health Center, WHI-Women Health Initiative, KMIC-Korean Medical Insurance Corporation, M-Men, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
The results in the literature show that the association between smoking and diabetes increases with an increase in the number of cigarettes smoked/day. Will et al. [63] analyzed the impact of gender on this association and showed that the association between cigarette smoking and type 2 diabetes is more in men compared to women. Similar results are obtained by Jee et al. [64] . Wannamethee et al. [65] revealed that an individual smoking pipe/cigar is 2.15 times more likely to develop type 2 diabetes and an individual smoking cigarette is 1.6 times more likely compared to a non-smoker. Kowall et al. [66] showed that the risk of incidence type 2 diabetes is significantly high in active/passive prediabetic smokers compared to active/passive smokers without prediabetes.
The incidence and prevalence of type 2 diabetes in ex-smokers is examined by [67] , [68] , [69] , [70] , [71] , [72] . and [73] respectively. Results show that ex-smokers are associated with 17–60% increased risk of type 2 diabetes [67] , [68] , [70] , [71] , [72] . However, the results obtained by Simon et al. [73] and Manson et al. [69] showed no association between ex-smokers and type 2 diabetes. This discrepancy in the results can be due to the heterogeneous characteristics (sample size, age range, men/women ratio and ethnicity) of the cohorts used in these studies. Beziaud et al. [74] examined gender-based prevalence of type 2 diabetes in ex-smokers and showed that women are at higher risk compared to men. Furthermore, the duration of smoking cessation also impacts the association in ex-smokers [65] , [75] , [76] , [77] . An individual is at high risk of developing type 2 diabetes during first 5–10 years of smoking cessation. The risk then decreases with an increase in cessation duration. The association between smoking cessation and the incidence of type 2 diabetes is more in women than men [78] .
In summary, both active and passive smoking are strongly associated with the incidence of type 2 diabetes. The association is more in men compared to women. Moreover, the association remains significant in ex-smokers during first the 5–10 years of smoking. After 10 years of smoking cessation, the risk of incidence type 2 diabetes is the same as that in a non-smoker. Women ex-smokers are at a higher risk of developing diabetes compared to men ex-smokers.
3.4. Depression
Depression is a mood disorder that negatively affects the way a person feels, thinks and acts [130] . It can be due to a family history of depression, early childhood trauma, brain structure, medical conditions, drug use or surrounding environment. Depression is associated with multiple health conditions including diabetes [131] . It elevates the sympathetic nervous system activities and hypothalamic–pituitary–adrenal axis activities [132] . Elevated sympathetic nervous system activities lead to an increase in catecholamines and inflammation, and eventually causing insulin resistance [133] . On the other hand, elevated adrenal axis activities lead to an increase in cortisol and eventually blood sugar level [134] . Both insulin resistance and increased blood sugar levels develop type 2 diabetes. The characteristics and findings of the work in the literature examining the association between depression and the incidence of type 2 diabetes are presented in Table 4 .
Characteristics and findings of the studies examining the association between depression and type 2 diabetes.
RS-Random Sample, SDS-Self rating Depression Scale, ECAPS-Epidemiologic Catchment Area Program Survey, NHANES-National Health and Nutrition Examination Survey, ARIC-Atherosclerosis Risk in Communities, RNH-RegistratieNet Huisarts Praktijken, SWAN-Study of Womens’ Health Across the Nation, NTHS-Nord Trondelag Health Study, CHS-Cardiovascular Health Study, CESD-Center for Epidemiological Studies Depression Scale, RBHCDS-Rancho Bernardo Heart and Chronic Disease Study, BDI-Beck Depression Inventory, M-Men, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
The results show that depression is highly associated with the incidence of type 2 diabetes. In the context of gender, depressed men are at higher risk of incidence type 2 diabetes, whereas depression in women is not associated with type 2 diabetes [135] . Moreover, compared to Caucasian, Hispanic, Japanese-American and Chinese-American, depressed African-Americans are at 2.56 times higher risk of incidence type 2 diabetes [136] . Based on self rating depression scale (SDS) score, an individual having a score of 48–80 is at higher risk of developing diabetes compared to an individual having a score of 20–39 [137] . Similarly, an individual having a score ⩾ 11 using center for epidemiological studies depression scale (CES-D) or a score ⩾ 8 using beck depression inventory (BDI) is at higher risk of incidence type 2 diabetes [138] , [139] .
In summary, depression is associated with type 2 diabetes. However, the association is different in men and women. Moreover, the study by Yu et al. [140] show that depression itself is not a risk factor for diabetes, rather the activities related to depression such as physical inactivity, poor diet, and obesity lead to diabetes. In addition, the medical drugs used to treat depression also have an association with the incidence of type 2 diabetes. Consequently, similar to high-level serum uric acid, depression is not an independent risk factor but it emphasizes the impact of other independent risk factors such as gender, ethnicity, physical inactivity, and obesity.
3.5. Cardiovascular disease
Increased heart rate and cardiovascular disease can elevate the blood pressure in the arteries. As a result, the body’s glucose uptake decreases leading to insulin resistance condition. Consequently, a person suffering from heart disease is at a higher risk of developing type 2 diabetes. However, this association is still obscure. Few studies argue that a history of cardiovascular disease leads to the incidence of type 2 diabetes [141] , while others claim that type 2 diabetes increases the risk of cardiovascular disease [142] , [143] , [144] . Yeung et al. [141] examined the association between family history of coronary heart disease (CHD) and type 2 diabetes ( Table 5 ). The authors concluded that a high family CHD score is associated to the incidence of type 2 diabetes in individuals who have a positive history of family diabetes. For the individuals having a negative family history of diabetes, this association was non-significant. In summary, it is debatable whether cardiovascular disease is a risk factor for type 2 diabetes or not.
Characteristics and findings of the studies examining the association between cardiovascular disease and type 2 diabetes.
ARIC-Atherosclerosis Risk in Communities, CDH-Coronary Heart Disease, M-Men, W-Women, PCS-Prospective Cohort Study.
3.6. Dyslipidemia
Dyslipidemia refers to an abnormal level of lipids, such as triglycerides and cholesterol. It is characterized by high triglyceride levels, increased low-density lipoproteins (LDL) levels and decreased high-density lipoproteins (HDL) levels [145] . Elevated LDL and lowered HDL levels lead to beta-cell dysfunction inhibiting insulin secretion and consequently type 2 diabetes [146] , [147] . Table 6 shows the characteristics and findings of the work in the literature studying the association between dyslipidemia and type 2 diabetes.
Characteristics and findings of the studies examining the association between dyslipidemia and type 2 diabetes.
LWHS-Lowa Women’s Health Study, CCHS-Copenhagen City heart Study, CGPS-Copenhagen General Population Study, MA-Meta Analysis, REACTION-Risk Evaluation of cAncers in Chinese diabeTic Individuals: a lONgitudinal study, RS-Random Sample, M-Men, W-Women, PCS-Prospective Cohort Study.
Dietary fats, that raise the total cholesterol and LDL levels, are considered significant in the development of type 2 diabetes [148] . Substituting saturated fatty acid with polyunsaturated fatty acid and animal fat with vegetable fat can help lower blood cholesterol and eventually type 2 diabetes. This is because both polyunsaturated fatty acid and vegetable fat are inversely related to the risk of incidence type 2 diabetes with RR 0.84 (95% CI 0.71–0.98) and RR 0.78 (95% CI 0.67–0.91) respectively for the highest quintile of intake [148] . Tajima et al. [149] also confirmed the association between high cholesterol diet intake ( > 273 mg/day) and type 2 diabetes (RR 1.25, 95% CI 1.16–1.36) compared to low cholesterol intake ( < 185 mg/day).
In order to reduce elevated LDL level, LDL lowering therapy and drugs are suggested. However, these drugs and therapy are found to be associated with a higher risk of type 2 diabetes [150] . Individuals having familial hypercholesterolemia, a genetic disorder that results in high LDL levels, are less likely to have type 2 diabetes compared to individuals having high LDL levels due to dietary patterns [151] . Zhang et al. [152] in their analysis found that the ratio of non-HDL and HDL levels is an independent risk factor for incidence diabetes. They show that an individual having a ratio of 3.1 is at 40% increased risk of incidence diabetes (OR 1.4, 95% CI 1.1–1.8) compared to an individual having a ratio of 1.4. Elevated non-HDL and lowered HDL levels are significantly associated with incidence diabetes [153] .
On the contrary to studies confirming the association between low-HDL levels and the incidence of type 2 diabetes, Haase et al. [154] in their study concluded that a life-long reduction in HDL levels are not associated with an increased risk of type 2 diabetes. They found that the association is most likely reverse causation, i.e., type 2 diabetes leads to low HDL levels.
3.7. Hypertension
Hypertension, also known as high blood pressure, is a medical condition in which the blood pressure in the arteries is persistently elevated. Hypertension elevates the sympathetic nervous system activity leading to a decrease in the body’s glucose uptake. This causes the condition of insulin resistance and eventually type 2 diabetes. Hypertension elevates sympathetic nervous system activities leading to impaired vasodilation of skeletal muscles. Consequently, muscle glucose uptake decreases with the eventual development of type 2 diabetes. Table 7 shows the characteristics and findings of the work in the literature studying the association between hypertension and type 2 diabetes.
Characteristics and findings of the studies examining the association between hypertension and type 2 diabetes.
RS-Random Sample, ARIC-Atherosclerosis Risk in Communities, WHS, Women’s Health Study, CARDIA-Coronary Artery Risk Development in Young Adults, FHS-Framingham Heart Study, GPPS-Gothenburg Primary Prevention Study, KGES-Korean Genome and Epidemiology Study, M-Men, W-Women, PCS-Prospective Cohort Study.
Hayashi et al. [166] examined the association between high normal blood pressure ( ⩾ 130 and < 140 mmHg/ ⩾ 85 and < 90) and hypertension ( ⩾ 140 mmHg/ ⩾ 90 mmHg), and the incidence of type 2 diabetes in men. The authors concluded that both high normal blood pressure (RR 1.39, 95%1.14–1.69) and hypertension (RR 1.75, 95% CI 1.43–2.16) are associated with an increased risk of type 2 diabetes. This association is dependent on obesity and hypertension medications. Hypertension medications are considered to increase the risk of diabetes depending on the type of medication [167] . For instance, hypertensive individuals taking thiazide diuretics and angiotensin-converting-enzyme medications are at lower risk of diabetes compared to the hypertensive individuals not taking any medication. However, those taking beta-blockers medication are at 28% higher risk of incidence type 2 diabetes (HR 1.28, 95% CI 1.04–1.57) [167] . The association between hypertension and the incidence of type 2 diabetes is significant in women as well [168] . Women having hypertension are at 2 times increased risk of developing diabetes (HR 2.03, 95% CI 1.77–2.32) compared to women having normal blood pressure ( < 120/75) [168] . The association is more in overweight and obese women. Irrespective of gender, prehypertension (HR 1.27, 95%CI 1.09–1.48) and hypertension (HR 1.51, 95% CI 1.29–1.76) are associated with increased risk of incidence type 2 diabetes [169] . In the context of ethnicity, whites individuals having hypertension are at higher risk of developing diabetes (HR 1.25, 95% CI 1.03–1.53), but no such association is seen in African American hypertensive individuals (HR 0.92, 95% CI 0.70–1.21) [170] .
In summary, hypertension is associated with the development of type 2 diabetes in both men and women. However, the association is ethnicity-dependent. The selection of hypertensive medications should be made properly as the medication impacts the strength of the association. Furthermore, an obese individual with hypertension is at higher risk compared to a non-obese.
The number of elderly people (above 60 years) is increasing worldwide. The 900 million global elderly population in 2015 is expected to rise to 2 billion by 2050 [171] . Aging increases the risk of metabolic syndrome and chronic diseases including type 2 diabetes. Aging increases chronic inflammation in an elderly individual leading to insulin resistance [172] . In addition, lipid metabolism disorder due to aging increases the accumulation of body fat leading to elevated free fatty acids concentration in the blood/plasma and eventually insulin resistance [173] . Consequently, an aged individual is at higher risk of developing type 2 diabetes. However, there is not much work concluding that aging is an independent risk factor for type 2 diabetes. Choi et al. [174] concluded that the risk of diabetes increases with aging only in overweight individuals, and the risk decreases with a moderate level of physical activity. Aging can be considered as triggering the association between independent risk factors and risk of diabetes, but more evidence and studies are required to examine the association between aging as an independent factor and diabetes.
3.9. Ethnicity
Ethnicity is associated with a range of health complications including diabetes because of the heterogeneity in the demographic environmental conditions and lifestyle. It is an independent risk factor which tends to be exacerbated by the social disadvantage and the affluent way of living. Table 8 shows the characteristics and findings of the work in the literature studying the association between ethnicity and type 2 diabetes. Compared to white individuals, type 2 diabetes is more prevalent in Pacific Islanders (OR 3.1, 95% CI 1.4–6.8), followed by Blacks (OR 2.3, 95% CI 2.1–2.6), Native Americans (OR 2.2, 95% CI 1.6–2.9), Hispanics (OR 2.0, 95% CI 1.8–2.3), and Multiracial (OR 1.8, 95% CI 1.5–2.9) [175] . In another study by Shai et al. [176] , it was found that compared to whites, Asians (RR 1.94, 95% CI 1.46–2.58), Hispanics (RR 1.70, 95% CI 1.28–2.26), and Blacks (RR 1.36, 95% CI 1.14–1.63) are at higher risk of incidence type 2 diabetes.
Characteristics and findings of the studies examining the association between ethnicity and type 2 diabetes.
RS-Random Sample, BRFSS-Behavioral Risk Factor Surveillance System, NHS-Nurses’ Health Study, PCS-Prospective Cohort Study.
A study by Zimmet et al. [177] showed that type 2 diabetes is 10 times more prevalent in rural Indians compared to rural Melanesians, and 2 times more prevalent in urban Indians compared to urban Melanesians. They also revealed that the prevalence is 5 times more in urban Melanesians compared to rural Melanesians. One of the reason could be that the rural residents have an increased amount of physical activity compared to the urban ones, leading to decreased risk of diabetes [178] . It should thus important to have a moderate amount of physical activity as a therapy for diabetes prevention. Compared to Europeans, type 2 diabetes is 3.8 times more prevalent in Indians, and the prevalence increases to 5 times for 40–64 years old individuals [179] . In another comparison between Asian and non-Asian ethnicity, it is found that the prevalence of type 2 diabetes in Bangladeshis (Asians) is more [180] . Furthermore, the prevalence is high in women (5.75 times) compared to that in men (2.2 times). However, ethnicity can not be considered as an independent risk factor for this association as Bangladeshis had higher smoking rates and a lower ratio of polyunsaturated fatty acids to saturated fatty acids. Consequently, ethnicity, smoking and dyslipidemia all contributed to the risk of incidence type 2 diabetes. Simmons et al. [181] also confirmed in their study that the prevalence is more in Asians compared to Whites. However, in contrast to the results obtained by [180] , Simmons et al. [181] found that the prevalence is more in men compared to women. This inconsistency should be examined further.
In summary, ethnicity is associated with the incidence of type 2 diabetes. However, there is no definite explanation of why individuals of a particular ethnicity are at higher risk of type 2 diabetes compared to the others. One possible explanation can be the ethnicity-dependent relation between BMI and body fat. For instance, Asians have around 3–4 kg/ m 2 lower BMI compared to Caucasians for a given percentage of body fat [182] . Another reason could be ethnicity-based insulin sensitivity. Studies show that Asians, Blacks and Mexican Americans are less insulin sensitive compared to non-Hispanic Whites [183] , [184] .
3.10. Family history of diabetes
Family history information can serve as a useful tool for prognosis/diagnosis and public health. Family history of diabetes reflects both genetic as well as environmental factors and can lead to better prediction of incidence type 2 diabetes than only genetic factors and environmental factors alone [192] . Table 9 shows the characteristics and findings of the work in the literature studying the association between family history of diabetes and type 2 diabetes.
Characteristics and findings of the studies examining the association between family history of diabetes and type 2 diabetes.
RS-Random Sample, SAHS-San Antonio Heart Study, MRFIT-Multiple Risk Factor Intervention Trial, MA-Meta Analysis, THHP-The Honolulu Heart Program, EPIC-European Prospective Investigation into Cancer, FHS-Framingham Heart Study, MONICA-Multinational MONItoring of trends and determinants in CArdiovascular disease, NHANES-National Health and Nutrition Examination Survey, PD-Prediabetes, IFG-Impaired Fasting Glucose, IGT-Impaired Glucose Tolerance, M-Men, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
A study by Tsenkova et al. [193] revealed that a family history of diabetes is strongly associated with incidence diabetes (OR 2.77, 95% CI 2.03–3.78). Another study also shows that parental history of diabetes is an independent risk factor for diabetes (OR 1.73, 95% CI 1.29–2.33) [194] . However, the association becomes weaker in men free of cardiovascular disease (OR 1.63, 95% CI 1.18-.2.24). Moreover, the association is much higher in 45–54 years old men (OR 1.99, 95% CI 1.38–2.89) compared to 55–68 years old men (OR 1.33, 95% CI 0.70–2.52). Furthermore, the prevalence of type 2 diabetes is stronger in men compared to women [195] . This indicates that parental history of diabetes in combination with other risk factors such as aging, gender and cardiovascular diseases, increases the risk of incidence type 2 diabetes.
Rodríguez-Moran et al. [196] showed that a family history of diabetes in first degree of relative (parents, offspring and siblings) is a strong and independent risk factor for the prevalence of impaired fasting glucose (prediabetes) (OR 11.7, 95% 9.5–21.2) in children and adolescents. This is in the absence of obesity. The results reveal that is it important to consider the parental history of diabetes while screening for diabetes children and adolescents. This is because only obesity-based screening could lead to underestimation. Valdez et al. [197] also showed that the family history of diabetes in at least two first-degree relatives or one first-degree and at least two second-degree relatives is significant for prevalence of type 2 diabetes. However, it can not be denied that the presence of a family history of diabetes can make the association between obesity and diabetes stronger [198] . Given a BMI ⩾ 35, an individual with a family history of diabetes is at a higher risk of incidence diabetes (OR 26.7, 95% CI 14.4–49.4) compared to the one without a family history of diabetes (OR 6.1, 95% CI3.4–11.2). Furthermore, ethnicity is also considered an important factor in an obese individual with a family history of diabetes [199] , [200] .
An individual having a family history of diabetes can have an early onset of diabetes compared to the ones without a family history. However, it is hard to conclude that which among the maternal, paternal and both maternal and paternal family history of diabetes is more significant for incidence/prevalence of type 2 diabetes as the results in the literature are inconsistent [195] , [201] , [202] , [203] , [204] , [205] .
3.11. Obesity
Obesity is a complex health condition that involves an excessive amount of body fat. It is defined by the BMI and further evaluated in terms of fat distribution via the waist-hip ratio. Abdominal fat in the body increases inflammation which decreases insulin sensitivity by disrupting the function of beta-cells. The insulin resistance condition then leads to the prevalence of type 2 diabetes. Table 10 shows the characteristics and findings of the work in the literature studying the association between obesity and type 2 diabetes.
Characteristics and findings of the studies examining the association between obesity and type 2 diabetes.
SWHS-Shanghai Women’s Health Study, BWHS- Black Women’s Health Study, RS-Random Sample, WC-Waist Circumference, TLGS-Tehran Lipid and Glucose Study, MAHES-Massachusetts Hispanic Elderly Study, H-Hispanics, NH-Non Hispanics, M-Men, W-Women, PCS-Prospective Cohort Study, CSS-Cross-Sectional Study.
Ishikawa-Takata et al. [206] found that the risk of diabetes increases significantly for an individual having a BMI greater than 29 kg/ m 2 . The relative risk of diabetes increases up to 38.8 (95% CI 31.9–47.2) for an individual having a BMI greater than 34.9 kg/ m 2 [119] . Furthermore, study shows that the association between obesity and incidence diabetes is gender-dependent [207] . For each 2 kg/ m 2 lower BMI, men are at 23% (15–30%) lower risk of diabetes, whereas women are at 27% (23–32%) lower risk. Further, the association between obesity and diabetes is also dependent on ethnicity [207] . For each 2 kg/ m 2 lower BMI, Asians are at 37% (26–46%) lower risk of diabetes, whereas Australians are at 25% (21–29%) lower risk.
Ohnishi et al. [208] found that compared to overall obesity, central obesity is highly associated with the risk of type 2 diabetes (RR 2.07, 95% CI 1.03–4.16). This association is more in elderly people ( ⩾ 60 years) (OR 3.8, 95% CI 1.8–7.7) [209] . The association between central obesity and the incidence of type 2 diabetes is found significant in both men and women. However, centrally obese women are at higher risk (OR 2.875, 95% CI 1.987–4.160) compared to centrally obese men (OR 2.308, 95% CI 1.473–3.615) [210] . The prevalence of type 2 diabetes in obese individual is ethnicity dependent [211] . Non-Hispanics centrally obese women are at higher risk of developing type 2 diabetes (OR 15.1, 95% CI 1.9–117.6) compared to centrally obese Hispanic women (OR 1.6, 95% CI 1.0–2.8). The centrally Hispanic men are also at risk of developing type 2 diabetes (OR 2.1, 95% CI 1.2–3.9). No such association is found in centrally obese Non-Hispanic men. However, all these studies examining the association between central obesity and the incidence of type 2 diabetes consider different definitions of central obesity. For instance, [208] defines central obesity as waist circumference (WC) ⩾ 85 cm in men and ⩾ 90 cm in women, whereas [211] defines it as WC > 102 cm in men and > 88 cm in women. Consequently, it is difficult to conclude the association between central obesity and the incidence of type 2 diabetes.
In summary, although obesity is a significant predictor, the association between obesity and diabetes is a factor of gender and ethnicity. Women with high BMI are at greater risk of diabetes compared to men. Moreover, the association is stronger in Asians compared to Australians. The association between central obesity is also found to be significant for the prevalence of type 2 diabetes. This association is the strongest in Non-Hispanics women. However, more studies are required to examine the association between central obesity and type 2 diabetes following one standard criterion defining central obesity.
3.12. Physical inactivity
An individual is considered physically inactive if he/she does not get the recommended 30–60 min of exercise three to four times a week. Physical inactivity decreases insulin sensitivity with progressive loss of beta-cells. This leads to impaired glucose tolerance and eventually type 2 diabetes. However, no work examines the association between physical inactivity as an independent factor and the prevalence of diabetes. One of the reasons that physical inactivity leads to type 2 diabetes can be that physical inactivity can cause obesity which in turn is a significant risk factor for type 2 diabetes.
4. Conclusion
Diabetes is a global crisis that is primarily driven by rapid urbanization, changing lifestyles, and uneven dietary patterns [215] , [216] . It is crucial to predict the prevalence of diabetes in an individual to reduce the risk of diabetes development and save lives. Diabetes is thought to prevail due to several risk factors such as high-level serum uric acid, sleep quality/quantity, smoking, depression, cardiovascular disease, dyslipidemia, hypertension, aging, ethnicity, family history of diabetes, physical inactivity, and obesity. Studies in the literature have examined the association between each of these risk factors and the risk of developing type 2 diabetes. In this review, we provide an analysis of the studies in the literature to deduce inferences on the relationship between the risk factors and incidence/prevalence of type 2 diabetes.
In conclusion, it can be observed that sleep quantity/quality, smoking, dyslipidemia, hypertension, ethnicity, family history of diabetes, obesity and physical inactivity are strongly associated with the development of type 2 diabetes. Both sleep quantity and quality are found to be strongly associated with the development of type 2 diabetes. The association is stronger in women sleeping for more hours and in men sleeping for fewer hours. However, the sleeping quantity and quality data in these studies are self-reported by the participants, and therefore, prone to errors. More studies are required that use measurement techniques for data collection to validate the association between sleep quantity/quality and type 2 diabetes. Smoking is also found to be a significant risk factor for type 2 diabetes. Both active and passive smokers are at higher risk of developing type 2 diabetes. Moreover, the risk for developing type 2 diabetes remains high in ex-smokers for the first 5–10 years of smoking cessation. Dyslipidemia is associated with the development of type 2 diabetes. Increased non-HDL and decreased HDL levels are strongly associated with type 2 diabetes. However, in the majority of these studies, the incidence or prevalence of type 2 diabetes is self-reported. Consequently, further studies are needed to validate this association between dyslipidemia and type 2 diabetes using standardized measurement techniques, such as A1C test [217] . Hypertension is a significant risk factor for type 2 diabetes and this is further elevated in obese individuals. Ethnicity strongly associates with the development of type 2 diabetes. This could be due to the fact that insulin sensitivity varies among individuals of different ethnicity. Family history of diabetes in first degree of relatives is strongly associated with the development of type 2 diabetes. In addition, family history of diabetes also signifies the association between obesity and type 2 diabetes. Obesity is found to a significant risk factor for incidence of type 2 diabetes and the association is stronger in women compared to men.
The association between serum uric acid and type 2 diabetes remains obscure. It can not be concluded that serum uric acid is an independent risk factor for type 2 diabetes or it only elevates the association between other independent risk factors such as obesity, hypertension, and dyslipidemia, and type 2 diabetes. Moreover, our analysis shows that there might be no association between serum uric acid and the development of type 2 diabetes, but rather there might be a reverse association, i.e., diabetes leads to elevated serum uric acid level. Similarly, based on the evidence in the literature, aging can not be considered as an independent risk factor for type 2 diabetes. Aging only emphasizes the association between obesity and type 2 diabetes. Depression as well is not found to an independent risk factor contributing to the development of type 2 diabetes. Rather, the activities related to depression such as physical inactivity, poor diet, and obesity leads to diabetes. There is no sufficient evidence to conclude the association between cardiovascular disease and type 2 diabetes. It is debatable whether cardiovascular disease leads to the development of type 2 diabetes. Consequently, more studies are required to study the direct association between these risk factors, i.e., serum uric acid, aging, depression, and cardiovascular disease, and incidence of type 2 diabetes.
Based on this study, we devise recommendations to different stakeholders leading to better patient care. In particular, we provide recommendations for allied healthcare professionals, individuals, and government institutions as follows:
Allied healthcare professionals: The hypertensive medications and the LDL lowering therapy and drugs should be carefully prescribed as they are associated with increased risk of type 2 diabetes. In addition, overweight and obese adults should be screened for diabetes.
Individuals: A healthy lifestyle, which involves intake of polyunsaturated fatty acids and vegetable fats, regular exercise, a healthy diet and proper sleep, is crucial. Individuals should avoid both active and passive smoking.
Government: Physical activity in the nation should be promoted for a healthy nation. Law policies should be implemented to restrict public smoking as passive smoking significantly increases the risk of type 2 diabetes. For instance, designated smoking areas can be established to eliminate the risk of developing passive smokers. It would be beneficial to have periodic surveys that include the demographic and lifestyle features of the citizens and the surveys’ results can be then used to develop a nation-wide diabetes prevention plan, in coordination with the allied health professionals.
CRediT authorship contribution statement
Leila Ismail: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing. Huned Materwala: Investigation, Writing - original draft. Juma Al Kaabi: Validation, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work is funded by the National Water and Energy Center of the United Arab Emirates University (Grant No. 31R215). We thank the anonymous reviewers for their valuable comments which helped us improve the paper.
Appendix A.
Search string used to retrieve the studies on the association between risk factor and type 2 diabetes.
Quality assessment of the included studies according to the Quality assessment tool for observational cohort and cross-sectional studies.
Q1. Was the research question or objective in this paper clearly stated?.
Q2. Was the study population clearly specified and defined?.
Q3. Was the participation rate of eligible persons at least 50%?
Q4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?.
Q5. Was a sample size justification, power description, or variance and effect estimates provided?.
Q6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?.
Q7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?.
Q8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)?.
Q9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?.
Q10. Was the exposure(s) assessed more than once over time?.
Q11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?.
Q12. Were the outcome assessors blinded to the exposure status of participants?.
Q13. Was loss to follow-up after baseline 20% or less?.
Q14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?.
CD-Cannot be Determined; NA-Not Applicable; NR-Not Reported.
- 1. Basics —diabetes— cdc. URL:https://www.cdc.gov/diabetes/basics/diabetes.html [Accessed on 03/05/2019].
- 2. The top 10 causes of death. URL:https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death [Accessed on 03/05/2019].
- 3. International diabetes federation – home. URL:https://idf.org/52-about-diabetes.html [Accessed on 03/06/2019].
- 4. C. for Disease Control, Prevention, et al. National diabetes statistics report: estimates of diabetes and its burden in the united states, 2014, Atlanta, GA: US Department of Health and Human Services; 2014.
- 5. 8940_idf_atlas_2017_english_interactive, URL:http://diabetesatlas.org/IDF_Diabetes_Atlas_8e_interactive_EN/, (Accessed on 03/06/2019).
- 6. Complications of diabetes. URL:https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444 [Accessed on 10/20/2020].
- 7. N.I. of Health. Study quality assessment tools, URL:https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools [Accessed on 02/27/2021].
- 8. Modan M., Halkin H., Karasik A., Lusky A. Elevated serum uric acid–a facet of hyperinsulinaemia. Diabetologia. 1987;30(9):713–718. doi: 10.1007/BF00296994. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Sautin YY, Nakagawa T, Zharikov S, Johnson RJ. Adverse effects of the classic antioxidant uric acid in adipocytes: Nadph oxidase-mediated oxidative/nitrosative stress. Am J Physiol Cell Physiol. [ DOI ] [ PubMed ]
- 10. Corry D.B., Eslami P., Yamamoto K., Nyby M.D., Makino H., Tuck M.L. Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin–angiotensin system. J Hypertension. 2008;26(2):269–275. doi: 10.1097/HJH.0b013e3282f240bf. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Kanellis J, Kang D-H. Uric acid as a mediator of endothelial dysfunction, inflammation, and vascular disease. In: Seminars in nephrology, vol. 25, Elsevier; 2005. p. 39–42. [ DOI ] [ PubMed ]
- 12. Johnson R.J., Nakagawa T., Sanchez-Lozada L.G., Shafiu M., Sundaram S., Le M., Ishimoto T., Sautin Y.Y., Lanaspa M.A. Sugar, uric acid, and the etiology of diabetes and obesity. Diabetes. 2013;62(10):3307–3315. doi: 10.2337/db12-1814. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Maedler K, Spinas GA, Lehmann R, Sergeev P, Weber M, Fontana A, Kaiser N, Donath MY. Glucose induces β -cell apoptosis via upregulation of the fas receptor in human islets. Diabetes 50 (8): 2001; 1683–1690. [ DOI ] [ PubMed ]
- 14. Perry I.J., Wannamethee S.G., Walker M.K., Thomson A., Whincup P.H., Shaper A.G. Prospective study of risk factors for development of non-insulin dependent diabetes in middle aged british men. BMJ. 1995;310(6979):560–564. doi: 10.1136/bmj.310.6979.560. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Niskanen L., Laaksonen D.E., Lindström J., Eriksson J.G., Keinänen-Kiukaanniemi S., Ilanne-Parikka P., Aunola S., Hämäläinen H., Tuomilehto J., Uusitupa M. Serum uric acid as a harbinger of metabolic outcome in subjects with impaired glucose tolerance: the finnish diabetes prevention study. Diabetes Care. 2006;29(3):709–711. doi: 10.2337/diacare.29.03.06.dc05-1465. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Dehghan A., Van Hoek M., Sijbrands E.J., Hofman A., Witteman J.C. High serum uric acid as a novel risk factor for type 2 diabetes. Diabetes Care. 2008;31(2):361–362. doi: 10.2337/dc07-1276. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Xu Y.-L., Xu K.-F., Bai J.-L., Liu Y., Yu R.-B., Liu C.-L., Shen C., Wu X.-H. Elevation of serum uric acid and incidence of type 2 diabetes: a systematic review and meta-analysis. Chronic Diseases Transl Med. 2016;2(2):81–91. doi: 10.1016/j.cdtm.2016.09.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Kodama S., Saito K., Yachi Y., Asumi M., Sugawara A., Totsuka K., Saito A., Sone H. Association between serum uric acid and development of type 2 diabetes. Diabetes Care. 2009;32(9):1737–1742. doi: 10.2337/dc09-0288. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Nakagawa T., Tuttle K.R., Short R.A., Johnson R.J. Hypothesis: fructose-induced hyperuricemia as a causal mechanism for the epidemic of the metabolic syndrome. Nat Rev Nephrol. 2005;1(2):80. doi: 10.1038/ncpneph0019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Herman J., Medalie J., Goldbourt U. Diabetes, prediabetes and uricaemia. Diabetologia. 1976;12(1):47–52. doi: 10.1007/BF01221964. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Chou P., Li C.-L., Wu G.-S., Tsai S.-T. Progression to type 2 diabetes among hign-risk groups in kin-chen, kinmen: exploring the natural history of type 2 diabetes. Diabetes Care. 1998;21(7):1183–1187. doi: 10.2337/diacare.21.7.1183. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Meisinger C., Thorand B., Schneider A., Stieber J., Döring A., Löwel H. Sex differences in risk factors for incident type 2 diabetes mellitus: the monica augsburg cohort study. Arch Internal Med. 2002;162(1):82–89. doi: 10.1001/archinte.162.1.82. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Carnethon M.R., Fortmann S.P., Palaniappan L., Duncan B.B., Schmidt M.I., Chambless L.E. Risk factors for progression to incident hyperinsulinemia: the atherosclerosis risk in communities study, 1987–1998. Am J Epidemiol. 2003;158(11):1058–1067. doi: 10.1093/aje/kwg260. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Chien K.-L., Chen M.-F., Hsu H.-C., Chang W.-T., Su T.-C., Lee Y.-T., Hu F.B. Plasma uric acid and the risk of type 2 diabetes in a chinese community. Clin Chem. 2008;54(2):310–316. doi: 10.1373/clinchem.2007.095190. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Nan H., Qiao Q., Söderberg S., Pitkäniemi J., Zimmet P., Shaw J., Alberti G., Uusitalo U., Pauvaday V., Chitson P. Serum uric acid and incident diabetes in mauritian indian and creole populations. Diabetes Res Clin Pract. 2008;80(2):321–327. doi: 10.1016/j.diabres.2008.01.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Choi H., De Vera M., Krishnan E. Gout and the risk of type 2 diabetes among men with a high cardiovascular risk profile. Rheumatology. 2008;47(10):1567–1570. doi: 10.1093/rheumatology/ken305. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Kramer C.K., Von Mühlen D., Jassal S.K., Barrett-Connor E. Serum uric acid levels improve prediction of incident type 2 diabetes in individuals with impaired fasting glucose: the rancho bernardo study. Diabetes Care. 2009;32(7):1272–1273. doi: 10.2337/dc09-0275. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Lv Q., Meng X.-F., He F.-F., Chen S., Su H., Xiong J., Gao P., Tian X.-J., Liu J.-S., Zhu Z.-H. High serum uric acid and increased risk of type 2 diabetes: a systemic review and meta-analysis of prospective cohort studies. PloS One. 2013;8(2) doi: 10.1371/journal.pone.0056864. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Taniguchi Y., Hayashi T., Tsumura K., Endo G., Fujii S., Okada K. Serum uric acid and the risk for hypertension and type 2 diabetes in japanese men: the osaka health survey. J Hypertension. 2001;19(7):1209–1215. doi: 10.1097/00004872-200107000-00005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Bandaru P., Shankar A. Association between serum uric acid levels and diabetes mellitus. Int J Endocrinol. 2011 doi: 10.1155/2011/604715. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Oda E., Kawai R., Sukumaran V., Watanabe K. Uric acid is positively associated with metabolic syndrome but negatively associated with diabetes in japanese men. Internal Med. 2009;48(20):1785–1791. doi: 10.2169/internalmedicine.48.2426. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Nan H., Dong Y., Gao W., Tuomilehto J., Qiao Q. Diabetes associated with a low serum uric acid level in a general chinese population. Diabetes Res Clin Pract. 2007;76(1):68–74. doi: 10.1016/j.diabres.2006.07.022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Facchini F., Chen Y.-D.I., Hollenbeck C.B., Reaven G.M. Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration. Jama. 1991;266(21):3008–3011. [ PubMed ] [ Google Scholar ]
- 34. Takada T., Kikuchi K., Hasegawa T., Komura H., Suzuki S., Satoh N., Ohotomo T., Nanba M., Marusaki S., Iimura O. The role of hyperinsulinemia on the renal mechanism of hyperuricemia in overweight patients with essential hypertension. Nihon Naibunpi Gakkai zasshi. 1991;67(8):861. doi: 10.1507/endocrine1927.67.8_861. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Investigators W.M.P.P. The world health organization monica project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol. 1988;41(2):105–114. doi: 10.1016/0895-4356(88)90084-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Investigators A. The atherosclerosis risk in communit (aric) study: design and objectives. Am J Epidemiol. 1989;129(4):687–702. [ PubMed ] [ Google Scholar ]
- 37. Eriksson J., Lindström J., Valle T., Aunola S., Hämäläinen H., Ilanne-Parikka P., Keinänen-Kiukaanniemi S., Laakso M., Lauhkonen M., Lehto P. Prevention of type ii diabetes in subjects with impaired glucose tolerance: the diabetes prevention study (dps) in finland study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia. 1999;42(7):793–801. doi: 10.1007/s001250051229. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Lee Y.-T., Lin R.S., Sung F.C., Yang C.-Y., Chien K.-L., Chen W.-J., Su T.-C., Hsu H.-C., Huang Y.-C. Chin-shan community cardiovascular cohort in taiwan–baseline data and five-year follow-up morbidity and mortality. J Clin Epidemiol. 2000;53(8):838–846. doi: 10.1016/s0895-4356(00)00198-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Hofman A., Grobbee D., De Jong P., Van den Ouweland F. Determinants of disease and disability in the elderly: the rotterdam elderly study. Eur J Epidemiol. 1991;7(4):403–422. doi: 10.1007/BF00145007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Group MRFIT, et al. Statistical design considerations in the nhli multiple risk factor intervention trial (mrfit). J Chronic Diseases 30 (5): 1977; 261–275. [ DOI ] [ PubMed ]
- 41. Group MRFITR, et al. Multiple risk factor intervention trial: risk factor changes and mortality results. Jama 248: 1982; 1465–1477. [ PubMed ]
- 42. Sherwin R., Kaelber C.T., Kezdi P., Kjelsberg M.O., Thomas H.E., Jr The multiple risk factor intervention trial (mrfit).: Ii. The development of the protocol. Prevent Med. 1981;10(4):402–425. doi: 10.1016/0091-7435(81)90058-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 43. Nchs – analytic and reporting guidelines: Nhanes iii. URL: https://www.cdc.gov/nchs/data/nhanes/nhanes3/nh3gui.pdf [Accessed on 02/26/2019].
- 44. Nhanes – nhanes iii – manuals and reports. URL: https://www.cdc.gov/nchs/nhanes/nh3rrm.htm [Accessed on 02/26/2019].
- 45. Bonnet M.H., Arand D.L. We are chronically sleep deprived. Sleep. 1995;18(10):908–911. doi: 10.1093/sleep/18.10.908. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Zizi F., Jean-Louis G., Brown C.D., Ogedegbe G., Boutin-Foster C., McFarlane S.I. Sleep duration and the risk of diabetes mellitus: epidemiologic evidence and pathophysiologic insights. Curr Diabetes Rep. 2010;10(1):43–47. doi: 10.1007/s11892-009-0082-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Fletcher E.C. Effect of episodic hypoxia on sympathetic activity and blood pressure. Respir Physiol. 2000;119(2–3):189–197. doi: 10.1016/s0034-5687(99)00114-0. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Punjabi N.M., Shahar E., Redline S., Gottlieb D.J., Givelber R., Resnick H.E. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the sleep heart health study. Am J Epidemiol. 2004;160(6):521–530. doi: 10.1093/aje/kwh261. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Shoelson S.E., Lee J., Goldfine A.B. Inflammation and insulin resistance. J Clin Investig. 2006;116(7):1793–1801. doi: 10.1172/JCI29069. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Björkelund C., Bondyr-Carlsson D., Lapidus L., Lissner L., Månsson J., Skoog I., Bengtsson C. Sleep disturbances in midlife unrelated to 32-year diabetes incidence: the prospective population study of women in gothenburg. Diabetes Care. 2005;28(11):2739–2744. doi: 10.2337/diacare.28.11.2739. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Von Ruesten A., Weikert C., Fietze I., Boeing H. Association of sleep duration with chronic diseases in the european prospective investigation into cancer and nutrition (epic)-potsdam study. PloS One. 2012;7(1) doi: 10.1371/journal.pone.0030972. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Mallon L., Broman J.-E., Hetta J. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28(11):2762–2767. doi: 10.2337/diacare.28.11.2762. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Zizi F., Pandey A., Murrray-Bachmann R., Vincent M., McFarlane S., Ogedegbe G., Jean-Louis G. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the national health interview survey. Am J Med. 2012;125(2):162–167. doi: 10.1016/j.amjmed.2011.08.020. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. Jackson C.L., Redline S., Kawachi I., Hu F.B. Association between sleep duration and diabetes in black and white adults. Diabetes Care. 2013;36(11):3557–3565. doi: 10.2337/dc13-0777. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Beihl D.A., Liese A.D., Haffner S.M. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009;19(5):351–357. doi: 10.1016/j.annepidem.2008.12.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Kawakami N., Takatsuka N., Shimizu H. Sleep disturbance and onset of type 2 diabetes. Diabetes Care. 2004;27(1):282–283. doi: 10.2337/diacare.27.1.282. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Nilsson P.M., Rööst M., Engström G., Hedblad B., Berglund G. Incidence of diabetes in middle-aged men is related to sleep disturbances. Diabetes Care. 2004;27(10):2464–2469. doi: 10.2337/diacare.27.10.2464. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Hayashino Y., Fukuhara S., Suzukamo Y., Okamura T., Tanaka T., Ueshima H. Relation between sleep quality and quantity, quality of life, and risk of developing diabetes in healthy workers in japan: the high-risk and population strategy for occupational health promotion (hipop-ohp) study. BMC Public Health. 2007;7(1):129. doi: 10.1186/1471-2458-7-129. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 59. Meisinger C., Heier M., Loewel H. Sleep disturbance as a predictor of type 2 diabetes mellitus in men and women from the general population. Diabetologia. 2005;48(2):235–241. doi: 10.1007/s00125-004-1634-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Tobacco. URL: https://www.who.int/news-room/fact-sheets/detail/tobacco [Accessed on 09/28/2020].
- 61. Smoking and diabetes — overviews of diseases/conditions. URL: https://www.cdc.gov/tobacco/campaign/tips/diseases/diabetes.html [Accessed on 10/20/2020].
- 62. Bajaj M. Nicotine and insulin resistance: when the smoke clears. Diabetes. 2012;61(12):3078–3080. doi: 10.2337/db12-1100. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 63. Will J.C., Galuska D.A., Ford E.S., Mokdad A., Calle E.E. Cigarette smoking and diabetes mellitus: evidence of a positive association from a large prospective cohort study. Int J Epidemiol. 2001;30(3):540–546. doi: 10.1093/ije/30.3.540. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Jee S.H., Foong A.W., Hur N.W., Samet J.M. Smoking and risk for diabetes incidence and mortality in korean men and women. Diabetes Care. 2010;33(12):2567–2572. doi: 10.2337/dc10-0261. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Wannamethee S.G., Shaper A.G., Perry I.J. Smoking as a modifiable risk factor for type 2 diabetes in middle-aged men. Diabetes CCare. 2001;24(9):1590–1595. doi: 10.2337/diacare.24.9.1590. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Kowall B., Rathmann W., Strassburger K., Heier M., Holle R., Thorand B., Giani G., Peters A., Meisinger C. Association of passive and active smoking with incident type 2 diabetes mellitus in the elderly population: the kora s4/f4 cohort study. Eur J Epidemiol. 2010;25(6):393–402. doi: 10.1007/s10654-010-9452-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Rimm E.B., Manson J.E., Stampfer M.J., Colditz G.A., Willett W.C., Rosner B., Hennekens C.H., Speizer F.E. Cigarette smoking and the risk of diabetes in women. Am J Public Health. 1993;83(2):211–214. doi: 10.2105/ajph.83.2.211. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 68. Rimm E.B., Chan J., Stampfer M.J., Colditz G.A., Willett W.C. Prospective study of cigarette smoking, alcohol use, and the risk of diabetes in men. BMJ. 1995;310(6979):555–559. doi: 10.1136/bmj.310.6979.555. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 69. Manson J.E., Ajani U.A., Liu S., Nathan D.M., Hennekens C.H. A prospective study of cigarette smoking and the incidence of diabetes mellitus among us male physicians. Am J Med. 2000;109(7):538–542. doi: 10.1016/s0002-9343(00)00568-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 70. Foy C.G., Bell R.A., Farmer D.F., Goff D.C., Wagenknecht L.E. Smoking and incidence of diabetes among us adults: findings from the insulin resistance atherosclerosis study. Diabetes Care. 2005;28(10):2501–2507. doi: 10.2337/diacare.28.10.2501. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Cho N.H., Chan J.C., Jang H.C., Lim S., Kim H.L., Choi S.H. Cigarette smoking is an independent risk factor for type 2 diabetes: a four-year community-based prospective study. Clin Endocrinol. 2009;71(5):679–685. doi: 10.1111/j.1365-2265.2009.03586.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Zhang L., Curhan G.C., Hu F.B., Rimm E.B., Forman J.P. Association between passive and active smoking and incident type 2 diabetes in women. Diabetes Care. 2011;34(4):892–897. doi: 10.2337/dc10-2087. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Simon J.A., Seeley D.G., Lipschutz R.C., Vittinghoff E., Browner W.S. The relation of smoking to waist-to-hip ratio and diabetes mellitus among elderly women. Prevent Med. 1997;26(5):639–644. doi: 10.1006/pmed.1997.0230. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Beziaud F., Halimi J., Lecomte P., Vol S., Tichet J. Cigarette smoking and diabetes mellitus. Diabetes Metab. 2004;30(2):161–166. doi: 10.1016/s1262-3636(07)70102-7. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Yeh H.-C., Duncan B.B., Schmidt M.I., Wang N.-Y., Brancati F.L. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Ann Internal Med. 2010;152(1):10–17. doi: 10.7326/0003-4819-152-1-201001050-00005. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. Morimoto A., Ohno Y., Tatsumi Y., Nishigaki Y., Maejima F., Mizuno S., Watanabe S. Impact of smoking cessation on incidence of diabetes mellitus among overweight or normal-weight japanese men. Diabetes Res Clin Pract. 2012;96(3):407–413. doi: 10.1016/j.diabres.2012.03.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Hur N.W., Kim H.C., Mo Nam C., Ha Jee S., Lee H.C., Suh I. Smoking cessation and risk of type 2 diabetes mellitus: Korea medical insurance corporation study. Eur J Cardiovasc Prevent Rehab. 2007;14(2):244–249. doi: 10.1097/01.hjr.0000239474.41379.79. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Oba S., Noda M., Waki K., Nanri A., Kato M., Takahashi Y., Poudel-Tandukar K., Matsushita Y., Inoue M., Mizoue T. Smoking cessation increases short-term risk of type 2 diabetes irrespective of weight gain: the japan public health center-based prospective study. PloS One. 2012;7(2) doi: 10.1371/journal.pone.0017061. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Ayas N.T., White D.P., Al-Delaimy W.K., Manson J.E., Stampfer M.J., Speizer F.E., Patel S., Hu F.B. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26(2):380–384. doi: 10.2337/diacare.26.2.380. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Colditz GA, Manson JE, Hankinson SE. The nurses’ health study: 20-year contribution to the understanding of health among women. J Women’s Health 6 (1): 1997; 49–62. [ DOI ] [ PubMed ]
- 81. Kawakami N., Takatsuka N., Shimizu H., Ishibashi H. Depressive symptoms and occurrence of type 2 diabetes among japanese men. Diabetes Care. 1999;22(7):1071–1076. doi: 10.2337/diacare.22.7.1071. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Nilsson P., Berglund G. Prevention of cardiovascular disease and diabetes: lessons from the malmö preventive project. J Internal Med. 2000;248(6):455–462. doi: 10.1046/j.1365-2796.2000.00766.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 83. Gottlieb D.J., Punjabi N.M., Newman A.B., Resnick H.E., Redline S., Baldwin C.M., Nieto F.J. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Internal Med. 2005;165(8):863–867. doi: 10.1001/archinte.165.8.863. [ DOI ] [ PubMed ] [ Google Scholar ]
- 84. Quan S.F., Howard B.V., Iber C., Kiley J.P., Nieto F.J., O’Connor G.T., Rapoport D.M., Redline S., Robbins J., Samet J.M. The sleep heart health study: design, rationale, and methods. Sleep. 1997;20(12):1077–1085. [ PubMed ] [ Google Scholar ]
- 85. Yaggi H.K., Araujo A.B., McKinlay J.B. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29(3):657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. O’donnell AB, Araujo AB, McKinlay JB. The health of normally aging men: the massachusetts male aging study (1987–2004). Exp Gerontol 39 (7): 2004; 975–984. [ DOI ] [ PubMed ]
- 87. Gangwisch J.E., Heymsfield S.B., Boden-Albala B., Buijs R.M., Kreier F., Pickering T.G., Rundle A.G., Zammit G.K., Malaspina D. Sleep duration as a risk factor for diabetes incidence in a large us sample. Sleep. 2007;30(12):1667–1673. doi: 10.1093/sleep/30.12.1667. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 88. Nhanes – national health and nutrition examination survey homepage, URL:https://www.cdc.gov/nchs/nhanes/index.htm [Accessed on 02/27/2019].
- 89. Chaput J.-P., Després J.-P., Bouchard C., Tremblay A. Association of sleep duration with type 2 diabetes and impaired glucose tolerance. Diabetologia. 2007;50(11):2298–2304. doi: 10.1007/s00125-007-0786-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 90. Bouchard C. Genetics of human obesity: recent results from linkage studies. J Nutr. 1997;127(9):1887S–1890S. doi: 10.1093/jn/127.9.1887S. [ DOI ] [ PubMed ] [ Google Scholar ]
- 91. Okamura T., Tanaka T., Babazono A., Yoshita K., Chiba N., Takebayashi T., Nakagawa H., Yamato H., Miura K., Tamaki J. The high-risk and population strategy for occupational health promotion (hipop-ohp) study: study design and cardiovascular risk factors at the baseline survey. J Human Hypertension. 2004;18(7):475. doi: 10.1038/sj.jhh.1001680. [ DOI ] [ PubMed ] [ Google Scholar ]
- 92. Tuomilehto H., Peltonen M., Partinen M., Seppä J., Saaristo T., Korpi-Hyövälti E., Oksa H., Puolijoki H., Saltevo J., Vanhala M. Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women–the fin-d2d survey. Sleep Med. 2008;9(3):221–227. doi: 10.1016/j.sleep.2007.04.015. [ DOI ] [ PubMed ] [ Google Scholar ]
- 93. Oy KH. Finnish diabetes association: Implementation of type 2 diabetes prevention plan, Helsinki 33.
- 94. Chaput J.-P., Després J.-P., Bouchard C., Astrup A., Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the quebec family study. Sleep Med. 2009;10(8):919–924. doi: 10.1016/j.sleep.2008.09.016. [ DOI ] [ PubMed ] [ Google Scholar ]
- 95. Wagenknecht L.E., Mayer E.J., Rewers M., Haffner S., Selby J., Borok G.M., Henkin L., Howard G., Savage P.J., Saad M.F. The insulin resistance atherosclerosis study (iras): objectives, design, and recruitment results. Ann Epidemiol. 1995;5(6):464–472. doi: 10.1016/1047-2797(95)00062-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 96. Vgontzas A.N., Liao D., Bixler E.O., Chrousos G.P., Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491–497. doi: 10.1093/sleep/32.4.491. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Tuomilehto H., Peltonen M., Partinen M., Lavigne G., Eriksson J.G., Herder C., Aunola S., Keinänen-Kiukaanniemi S., Ilanne-Parikka P., Uusitupa M. Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: the finnish diabetes prevention study. Diabetes Care. 2009;32(11):1965–1971. doi: 10.2337/dc08-1980. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Xu Q., Song Y., Hollenbeck A., Blair A., Schatzkin A., Chen H. Day napping and short night sleeping are associated with higher risk of diabetes in older adults. Diabetes Care. 2010;33(1):78–83. doi: 10.2337/dc09-1143. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. Schatzkin A., Subar A.F., Thompson F.E., Harlan L.C., Tangrea J., Hollenbeck A.R., Hurwitz P.E., Coyle L., Schussler N., Michaud D.S. Design and serendipity in establishing a large cohort with wide dietary intake distributions: the national institutes of health–american association of retired persons diet and health study. Am J Epidemiol. 2001;154(12):1119–1125. doi: 10.1093/aje/154.12.1119. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Chao C.-Y., Wu J.-S., Yang Y.-C., Shih C.-C., Wang R.-H., Lu F.-H., Chang C.-J. Sleep duration is a potential risk factor for newly diagnosed type 2 diabetes mellitus. Metabolism. 2011;60(6):799–804. doi: 10.1016/j.metabol.2010.07.031. [ DOI ] [ PubMed ] [ Google Scholar ]
- 101. Boeing H., Wahrendorf J., Becker N. Epic-germany–a source for studies into diet and risk of chronic diseases. Ann Nutr Metab. 1999;43(4):195–204. doi: 10.1159/000012786. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Kita T., Yoshioka E., Satoh H., Saijo Y., Kawaharada M., Okada E., Kishi R. Short sleep duration and poor sleep quality increase the risk of diabetes in japanese workers with no family history of diabetes. Diabetes Care. 2012;35(2):313–318. doi: 10.2337/dc11-1455. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 103. Massey JT, Moore TF, Tadros W, Parsons V. Design and estimation for the national health interview survey 1985–94. Vital Health Stat Series 2 Data Eval Methods Res (110): 1989; 1–33. [ PubMed ]
- 104. Najafian J., Mohamadifard N., Sadri G., Rahmati M. Association between sleep duration and diabetes mellitus: Isfahan healthy heart program. Nigerian J Clin Pract. 2013;16(1):59–62. doi: 10.4103/1119-3077.106756. [ DOI ] [ PubMed ] [ Google Scholar ]
- 105. Sarraf-Zadegan N., Sadri G., Malek-Afzali H., Baghaei M., Mohammadi-Fard N., Shahrokhi S., Tolooie H., Poormoghaddas M., Sadeghi M., Tavassoli A. Isfahan healthy heart programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control. design, methods and initial experience. Acta Cardiol. 2003;58(4):309–320. doi: 10.2143/AC.58.4.2005288. [ DOI ] [ PubMed ] [ Google Scholar ]
- 106. Boyko EJ, Seelig AD, Jacobson IG, Hooper TI, Smith B, Smith TC, Crum-Cianflone NF, MCS Team, et al. Sleep characteristics, mental health, and diabetes risk: a prospective study of us military service members in the millennium cohort study. Diabetes Care 36 (10): 2013; 3154–3161. [ DOI ] [ PMC free article ] [ PubMed ]
- 107. Ryan M.A., Smith T.C., Smith B., Amoroso P., Boyko E.J., Gray G.C., Gackstetter G.D., Riddle J.R., Wells T.S., Gumbs G. Millennium cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60(2):181–191. doi: 10.1016/j.jclinepi.2006.05.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 108. Holliday E.G., Magee C.A., Kritharides L., Banks E., Attia J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PloS One. 2013;8(11) doi: 10.1371/journal.pone.0082305. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 109. Banks E., Jorm L., Lujic S., Rogers K. Health, ageing and private health insurance: baseline results from the 45 and up study cohort. Aust New Zealand Health Policy. 2009;6(1):16. doi: 10.1186/1743-8462-6-16. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 110. Feskens E.J., Kromhout D. Cardiovascular risk factors and the 25-year incidence of diabetes mellitus in middle-aged men. Am J Epidemiol. 1989;130(6):1101–1108. doi: 10.1093/oxfordjournals.aje.a115437. [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Feinleib M. Seven countries: a multivariate analysis of death and coronary heart disease. Jama. 1981;245(5):511–512. [ Google Scholar ]
- 112. Kawakami N., Takatsuka N., Shimizu H., Ishibashi H. Effects of smoking on the incidence of non-lnsulin-dependent diabetes mellitus: replication and extension in a japanese cohort of male employees. Am J Epidemiol. 1997;145(2):103–109. doi: 10.1093/oxfordjournals.aje.a009080. [ DOI ] [ PubMed ] [ Google Scholar ]
- 113. Cummings S.R., Black D.M., Nevitt M.C., Browner W.S., Cauley J.A., Genant H.K., Mascioli S.R., Scott J.C., Seeley D.G., Steiger P. Appendicular bone density and age predict hip fracture in women. Jama. 1990;263(5):665–668. [ PubMed ] [ Google Scholar ]
- 114. Uchimoto S., Tsumura K., Hayashi T., Suematsu C., Endo G., Fujii S., Okada K. Impact of cigarette smoking on the incidence of type 2 diabetes mellitus in middle-aged japanese men: the osaka health survey. Diabet Med. 1999;16(11):951–955. doi: 10.1046/j.1464-5491.1999.00173.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 115. F.R. on the Aspirin Component of the Ongoing Physicians’ Health Study. Steering committee of the physicians’ health study research group. N Engl J Med 321 (3): 1989; 129–135. [ DOI ] [ PubMed ]
- 116. Ko G., Chan J., Tsang L., Critchley J., Cockram C. Smoking and diabetes in chinese men. Postgr Med J. 2001;77(906):240–243. doi: 10.1136/pmj.77.906.240. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 117. Shaper A., Pocock S., Walker M., Cohen N., Wale C., Thomson A. British regional heart study: cardiovascular risk factors in middle-aged men in 24 towns. Br Med J (Clin Res Ed) 1981;283(6285):179–186. doi: 10.1136/bmj.283.6285.179. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 118. Garfinkel L. Selection, follow-up, and analysis in the american cancer society prospective studies. Nat Cancer Inst Monograph. 1985;67:49–52. [ PubMed ] [ Google Scholar ]
- 119. Hu F.B., Manson J.E., Stampfer M.J., Colditz G., Liu S., Solomon C.G., Willett W.C. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. New England J Med. 2001;345(11):790–797. doi: 10.1056/NEJMoa010492. [ DOI ] [ PubMed ] [ Google Scholar ]
- 120. Montgomery S.M., Ekbom A. Smoking during pregnancy and diabetes mellitus in a british longitudinal birth cohort. BMJ. 2002;324(7328):26–27. doi: 10.1136/bmj.324.7328.26. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 121. Ekinsmyth C, Bynner J, Montgomery S, Shepherd P. An integrated approach to the design and analysis of the 1970 british cohort study (bcs70) and the national child development study (ncds). London: Centre for Longitudinal Studies, University of London
- 122. Carlsson S., Midthjell K., Grill V. Smoking is associated with an increased risk of type 2 diabetes but a decreased risk of autoimmune diabetes in adults: an 11-year follow-up of incidence of diabetes in the nord-trøndelag study. Diabetologia. 2004;47(11):1953–1956. doi: 10.1007/s00125-004-1554-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Midthjell K., Bjørndal A., Holmen J., Krüger Ø., Bjartveit K. Prevalence of known and previously unknown diabetes mellitus and impaired glucose tolerance in an adult norwegian population. indications of an increasing diabetes prevalence. the nord-trøndelag diabetes study. Scand J Primary Health Care. 1995;13(3):229–235. doi: 10.3109/02813439508996766. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Hyeon C.K., Chung M.N., Sun H.J., Kwang H.H., Oh D.K., Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328(7446):983. doi: 10.1136/bmj.38050.593634.63. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 125. Rathmann W, Haastert B, Icks AA, Löwel H, Meisinger C, Holle R, Giani G. High prevalence of undiagnosed diabetes mellitus in southern germany: target populations for efficient screening. The kora survey 2000. Diabetologia 46 (2): 2003; 182–189. [ DOI ] [ PubMed ]
- 126. Jee S.H., Ohrr H., Sull J.W., Yun J.E., Ji M., Samet J.M. Fasting serum glucose level and cancer risk in korean men and women. Jama. 2005;293(2):194–202. doi: 10.1001/jama.293.2.194. [ DOI ] [ PubMed ] [ Google Scholar ]
- 127. Tsugane S., Sobue T. Baseline survey of jphc study design and participation rate. J Epidemiol. 2001;11(6sup):24–29. doi: 10.2188/jea.11.6sup_24. [ DOI ] [ PubMed ] [ Google Scholar ]
- 128. Luo J., Rossouw J., Tong E., Giovino G.A., Lee C.C., Chen C., Ockene J.K., Qi L., Margolis K.L. Smoking and diabetes: does the increased risk ever go away? Am J Epidemiol. 2013;178(6):937–945. doi: 10.1093/aje/kwt071. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 129. Study TWHI, et al. Design of the women’s health initiative clinical trial and observational study, Controlled Clin Trials 19 (1): 1998; 61–109. [ DOI ] [ PubMed ]
- 130. What is depression? URL:https://www.psychiatry.org/patients-families/depression/what-is-depression [Accessed on 09/29/2020].
- 131. Jacobson A.M. Depression and diabetes. Diabetes Care. 1993;16(12):1621–1623. doi: 10.2337/diacare.16.12.1621. [ DOI ] [ PubMed ] [ Google Scholar ]
- 132. Plotsky P.M., Owens M.J., Nemeroff C.B. Psychoneuroendocrinology of depression: hypothalamic-pituitary-adrenal axis. Psychiatr Clin North Am. 1998;21(2):293–307. doi: 10.1016/s0193-953x(05)70006-x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 133. Mannelli M, Parenti G, Zampetti B, Canu L, Mannucci E. Diabetes from catecholamine excess. In: Diabetes secondary to endocrine and pancreatic disorders, vol. 22, Karger Publishers; 2014. p. 44–51.
- 134. Vreeburg S.A., Hoogendijk W.J., van Pelt J., DeRijk R.H., Verhagen J.C., van Dyck R., Smit J.H., Zitman F.G., Penninx B.W. Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: results from a large cohort study. Arch Gen Psychiatry. 2009;66(6):617–626. doi: 10.1001/archgenpsychiatry.2009.50. [ DOI ] [ PubMed ] [ Google Scholar ]
- 135. van den Akker M, Schuurman A, Metsemakers J, Buntinx F. Is depression related to subsequent diabetes mellitus? Acta Psychiatr Scand 110 (3): 2004; 178–183. arXiv:https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1600-0447.2004.00333.x, doi:10.1111/j.1600-0447.2004.00333.x. URL:https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0447.2004.00333.x. [ DOI ] [ PubMed ]
- 136. Everson-Rose SA, Meyer PM, Powell LH, Pandey D, Torréns JI, Kravitz HM, Bromberger JT, Matthews KA. Depressive symptoms, insulin resistance, and risk of diabetes in women at midlife. Diabetes Care 27 (12): 2004; 2856–2862. arXiv: http://care.diabetesjournals.org/content/27/12/2856.full.pdf, doi: 10.2337/diacare.27.12.2856. URL: http://care.diabetesjournals.org/content/27/12/2856. [ DOI ] [ PubMed ]
- 137. Kawakami N., Takatsuka N., Shimizu H., Ishibashi H. Depressive symptoms and occurrence of type 2 diabetes among japanese men. Diabetes Care. 1999;22(7):1071–1076. doi: 10.2337/diacare.22.7.1071. arXiv:http://care.diabetesjournals.org/content/22/7/1071.full.pdf URL:http://care.diabetesjournals.org/content/22/7/1071. [ DOI ] [ PubMed ] [ Google Scholar ]
- 138. Carnethon M.R., Biggs M.L., Barzilay J.I., Smith N.L., Vaccarino V., Bertoni A.G., Arnold A., Siscovick D. Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the cardiovascular health study. Arch Internal Med. 2007;167(8):802–807. doi: 10.1001/archinte.167.8.802. arXiv:https://jamanetwork.com/journals/jamainternalmedicine/articlepdf/412313/ioi70010_802_807.pdf URL:https://dx.doi.org/10.1001/archinte.167.8.802. [ DOI ] [ PubMed ] [ Google Scholar ]
- 139. Palinkas L., Lee P.P., Barrett-Connor E. A prospective study of type 2 diabetes and depressive symptoms in the elderly: the rancho bernardo study. Diab Med J Br Diabetic Assoc. 2004;21:1185–1191. doi: 10.1111/j.1464-5491.2004.01315.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 140. Yu M., Zhang X., Lu F., Fang L. Depression and risk for diabetes: a meta-analysis. Can J Diabetes. 2015;39(4):266–272. doi: 10.1016/j.jcjd.2014.11.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 141. Yeung E.H., Pankow J.S., Astor B.C., Powe N.R., Saudek C.D., Kao W.L. Increased risk of type 2 diabetes from a family history of coronary heart disease and type 2 diabetes. Diabetes Care. 2007;30(1):154–156. doi: 10.2337/dc06-1463. [ DOI ] [ PubMed ] [ Google Scholar ]
- 142. Laakso M. Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes. 1999;48(5):937–942. doi: 10.2337/diabetes.48.5.937. [ DOI ] [ PubMed ] [ Google Scholar ]
- 143. Mazzone T., Chait A., Plutzky J. Cardiovascular disease risk in type 2 diabetes mellitus: insights from mechanistic studies. The Lancet. 2008;371(9626):1800–1809. doi: 10.1016/S0140-6736(08)60768-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 144. Fox C.S. Cardiovascular disease risk factors, type 2 diabetes mellitus, and the framingham heart study. Trends Cardiovasc Med. 2010;20(3):90–95. doi: 10.1016/j.tcm.2010.08.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 145. Olsson A.G., Schwartz G.G., Szarek M., Sasiela W.J., Ezekowitz M.D., Ganz P., Oliver M.F., Waters D., Zeiher A. High-density lipoprotein, but not low-density lipoprotein cholesterol levels influence short-term prognosis after acute coronary syndrome: results from the miracl trial. Eur Heart J. 2005;26(9):890–896. doi: 10.1093/eurheartj/ehi186. [ DOI ] [ PubMed ] [ Google Scholar ]
- 146. Zheng T., Gao Y., Tian H. Relationship between blood lipid profiles and pancreatic islet β) cell function in chinese men and women with normal glucose tolerance: a cross-sectional study. BMC Public Health. 2012;12(1):634. doi: 10.1186/1471-2458-12-634. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 147. Kawamoto R., Tabara Y., Kohara K., Miki T., Kusunoki T., Takayama S., Abe M., Katoh T., Ohtsuka N. Relationships between lipid profiles and metabolic syndrome, insulin resistance and serum high molecular adiponectin in japanese community-dwelling adults. Lipids Health Disease. 2011;10(1):79. doi: 10.1186/1476-511X-10-79. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 148. Meyer K.A., Kushi L.H., Jacobs D.R., Folsom A.R. Dietary fat and incidence of type 2 diabetes in older iowa women. Diabetes Care. 2001;24(9):1528–1535. doi: 10.2337/diacare.24.9.1528. [ DOI ] [ PubMed ] [ Google Scholar ]
- 149. Tajima R., Kodama S., Hirata M., Horikawa C., Fujihara K., Yachi Y., Yoshizawa S., Iida K.T., Sone H. High cholesterol intake is associated with elevated risk of type 2 diabetes mellitus–a meta-analysis. Clin Nutr. 2014;33(6):946–950. doi: 10.1016/j.clnu.2014.03.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 150. Lotta L.A., Sharp S.J., Burgess S., Perry J.R., Stewart I.D., Willems S.M., Luan J., Ardanaz E., Arriola L., Balkau B. Association between low-density lipoprotein cholesterol–lowering genetic variants and risk of type 2 diabetes: a meta-analysis. Jama. 2016;316(13):1383–1391. doi: 10.1001/jama.2016.14568. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 151. Besseling J., Kastelein J.J., Defesche J.C., Hutten B.A., Hovingh G.K. Association between familial hypercholesterolemia and prevalence of type 2 diabetes mellitus. Jama. 2015;313(10):1029–1036. doi: 10.1001/jama.2015.1206. [ DOI ] [ PubMed ] [ Google Scholar ]
- 152. Zhang N., Hu X., Zhang Q., Bai P., Cai M., Zeng T.S., Zhang J.-Y., Tian S.-H., Min J., Huang H.-T., Zheng J., Peng M.-M., Li M.-J., Chen L.-L. Non-high-density lipoprotein cholesterol: high-density lipoprotein cholesterol ratio is an independent risk factor for diabetes mellitus: results from a population-based cohort study. J Diabetes. 2018;10(9):708–714. doi: 10.1111/1753-0407.12650. arXiv:https://onlinelibrary.wiley.com/doi/pdf/10.1111/1753-0407.12650 URL:https://onlinelibrary.wiley.com/doi/abs/10.1111/1753-0407.12650. [ DOI ] [ PubMed ] [ Google Scholar ]
- 153. Song Q., Liu X., Wang A., Wang Y., Zhou Y., Zhou W., Wang X. Associations between non-traditional lipid measures and risk for type 2 diabetes mellitus in a chinese community population: a cross-sectional study. Lipids health Disease. 2016;15(1):70. doi: 10.1186/s12944-016-0239-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 154. Haase C.L., Tybjærg-Hansen A., Nordestgaard B.G., Frikke-Schmidt R. Hdl cholesterol and risk of type 2 diabetes: a mendelian randomization study. Diabetes. 2015;64(9):3328–3333. doi: 10.2337/db14-1603. [ DOI ] [ PubMed ] [ Google Scholar ]
- 155. Eaton W.W., Armenian H., Gallo J., Pratt L., Ford D.E. Depression and risk for onset of type ii diabetes: a prospective population-based study. Diabetes Care. 1996;19(10):1097–1102. doi: 10.2337/diacare.19.10.1097. arXiv:http://care.diabetesjournals.org/content/19/10/1097.full.pdf URL:http://care.diabetesjournals.org/content/19/10/1097. [ DOI ] [ PubMed ] [ Google Scholar ]
- 156. Regier D.A., Myers J.K., Kramer M., Robins L.N., Blazer D.G., Hough R.L., Eaton W.W., Locke B.Z. The NIMH epidemiologic catchment area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934–941. doi: 10.1001/archpsyc.1984.01790210016003. arXiv:https://jamanetwork.com/journals/jamapsychiatry/articlepdf/493431/archpsyc_41_10_003.pdf URL:https://dx.doi.org/10.1001/archpsyc.1984.01790210016003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 157. Carnethon MR, Kinder LS, Fair JM, Stafford RS, Fortmann SP. Symptoms of depression as a risk factor for incident diabetes: findings from the National Health and Nutrition Examination epidemiologic follow-up study, 1971–1992. Am J Epidemiol 158 (5): 2003; 416–423. arXiv:http://oup.prod.sis.lan/aje/article-pdf/158/5/416/149380/kwg172.pdf, doi:10.1093/aje/kwg172. URL:https://dx.doi.org/10.1093/aje/kwg172. [ DOI ] [ PubMed ]
- 158. Golden SH, Williams JE, Ford DE, Yeh H-C, Paton Sanford C, Nieto FJ, Brancati FL. Depressive symptoms and the risk of type 2 diabetes. Diabetes Care 27 (2): 2004; 429–435. arXiv:http://care.diabetesjournals.org/content/27/2/429.full.pdf, doi:10.2337/diacare.27.2.429. URL:http://care.diabetesjournals.org/content/27/2/429. [ DOI ] [ PubMed ]
- 159. Fran M, Sowers R, Crawford S, Sternfeld B, Morganstein D, Gold EB, Greendale GA, Evans DA, Neer R, Matthews KA, Sherman S, Lo A, Weiss G, Kelsey JL. Swan: a multicenter, multiethnic, community-based cohort study of women and the menopausal transition, Sybil L. Crawford.
- 160. Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. J Psychosomat Res. 2007;62(1):31–38. doi: 10.1016/j.jpsychores.2006.07.009. URL:http://www.sciencedirect.com/science/article/pii/S002239990600331X. [ DOI ] [ PubMed ] [ Google Scholar ]
- 161. Fried L., Borhani N., Enright P., Furberg C., Gardin J., Kronmal R., Kuller L., Manolio T., Mittelmark M., Newman A., O’Leary D., Psaty B., Rautaharju P., Tracy R., Weiler P. The cardiovascular health study: design and rationale. Ann Epidemiol. 1991;1(3):263–276. doi: 10.1016/1047-2797(91)90005-W. [ DOI ] [ PubMed ] [ Google Scholar ]
- 162. Folsom A.R., Prineas R.J., Kaye S.A., Soler J.T. Body fat distribution and self-reported prevalence of hypertension, heart attack, and other heart disease in older women. Int J Epidemiol. 1989;18(2):361–367. doi: 10.1093/ije/18.2.361. [ DOI ] [ PubMed ] [ Google Scholar ]
- 163. Aguib Y, Al Suwaidi J. The copenhagen city heart study (Østerbroundersøgelsen). Global Cardiol Sci Pract 2015 (3): 2015; 33. doi:10.5339/gcsp.2015.33. URL:http://europepmc.org/articles/PMC4625209. [ DOI ] [ PMC free article ] [ PubMed ]
- 164. Bergholdt H., Bathum L., Kvetny J., Rasmussen D.B., Moldow B., Hoeg T., Jemec G., Berner-Nielsen H., Nordestgaard B.G., Ellervik C. Study design, participation and characteristics of the danish general suburban population study. Dan Med J. 2013;60(9):A4693. [ PubMed ] [ Google Scholar ]
- 165. Ning G, RS Group. Risk evaluation of cancers in chinese diabetic individuals: a longitudinal (reaction) study. J Diabetes 4 (2): 2012; 172–173 [ DOI ] [ PubMed ]
- 166. Hayashi T., Tsumura K., Suematsu C., Endo G., Fujii S., Okada K. High normal blood pressure, hypertension, and the risk of type 2 diabetes in japanese men. The osaka health survey. Diabetes Care. 1999;22(10):1683–1687. doi: 10.2337/diacare.22.10.1683. [ DOI ] [ PubMed ] [ Google Scholar ]
- 167. Gress T.W., Nieto F.J., Shahar E., Wofford M.R., Brancati F.L. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. New England J Med. 2000;342(13):905–912. doi: 10.1056/NEJM200003303421301. [ DOI ] [ PubMed ] [ Google Scholar ]
- 168. Conen D., Ridker P.M., Mora S., Buring J.E., Glynn R.J. Blood pressure and risk of developing type 2 diabetes mellitus: the women’s health study. Eur Heart J. 2007;28(23):2937–2943. doi: 10.1093/eurheartj/ehm400. [ DOI ] [ PubMed ] [ Google Scholar ]
- 169. Kim M.-J., Lim N.-K., Choi S.-J., Park H.-Y. Hypertension is an independent risk factor for type 2 diabetes: the korean genome and epidemiology study. Hypertension Res. 2015;38(11):783. doi: 10.1038/hr.2015.72. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 170. Wei G.S., Coady S.A., Goff D.C., Brancati F.L., Levy D., Selvin E., Vasan R.S., Fox C.S. Blood pressure and the risk of developing diabetes in african americans and whites: Aric, cardia, and the framingham heart study. Diabetes Care. 2011;34(4):873–879. doi: 10.2337/dc10-1786. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 171. Ageing and health. URL:https://www.who.int/news-room/fact-sheets/detail/ageing-and-health [Accessed on 09/30/2020].
- 172. Sarkar D., Lebedeva I.V., Emdad L., Kang D.-C., Baldwin A.S., Fisher P.B. Human polynucleotide phosphorylase (hpnpaseold-35): a potential link between aging and inflammation. Cancer Res. 2004;64(20):7473–7478. doi: 10.1158/0008-5472.CAN-04-1772. [ DOI ] [ PubMed ] [ Google Scholar ]
- 173. Suastika K, Dwipayana P, Semadi MS, Kuswardhani RT. Age is an important risk factor for type 2 diabetes mellitus and cardiovascular diseases. Glucose Tolerance: Intech Open 2012; 67–76
- 174. Choi B., Shi F. Risk factors for diabetes mellitus by age and sex: results of the national population health survey. Diabetologia. 2001;44(10):1221–1231. doi: 10.1007/s001250100648. [ DOI ] [ PubMed ] [ Google Scholar ]
- 175. McNeely M.J., Boyko E.J. Type 2 diabetes prevalence in asian americans: results of a national health survey. Diabetes Care. 2004;27(1):66–69. doi: 10.2337/diacare.27.1.66. [ DOI ] [ PubMed ] [ Google Scholar ]
- 176. Shai I., Jiang R., Manson J.E., Stampfer M.J., Willett W.C., Colditz G.A., Hu F.B. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29(7):1585–1590. doi: 10.2337/dc06-0057. [ DOI ] [ PubMed ] [ Google Scholar ]
- 177. Zimmet P., Taylor R., Ram P., King H., Sloman G., Raper L.R., Hunt D. Prevalence of diabetes and impaired glucose tolerance in the biracial (melanesian and indian) population of fiji: a rural-urban comparison. Am J Epidemiol. 1983;118(5):673–688. doi: 10.1093/oxfordjournals.aje.a113678. [ DOI ] [ PubMed ] [ Google Scholar ]
- 178. Zimmet P., Faaiuso S., Ainuu J., Whitehouse S., Milne B., DeBoer W. The prevalence of diabetes in the rural and urban polynesian population of western samoa. Diabetes. 1981;30(1):45–51. doi: 10.2337/diab.30.1.45. [ DOI ] [ PubMed ] [ Google Scholar ]
- 179. Mather H.M., Keen H. The southall diabetes survey: prevalence of known diabetes in asians and Europeans. Br Med J (Clin Res Ed) 1985;291(6502):1081–1084. doi: 10.1136/bmj.291.6502.1081. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 180. McKeigue P., Marmot M., Cottier D., Rahman S., Riemersma R. Diabetes, hyperinsulinaemia, and coronary risk factors in bangladeshis in east London. Heart. 1988;60(5):390–396. doi: 10.1136/hrt.60.5.390. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 181. Simmons D., Williams D., Powell M. Prevalence of diabetes in a predominantly asian community: preliminary findings of the coventry diabetes study. BMJ. 1989;298(6665):18–21. doi: 10.1136/bmj.298.6665.18. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 182. Deurenberg P., Deurenberg-Yap M., Guricci S. Asians are different from caucasians and from each other in their body mass index/body fat per cent relationship. Obesity Rev. 2002;3(3):141–146. doi: 10.1046/j.1467-789x.2002.00065.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 183. TORRens JI, Skurnick J, Davidow AL, Korenman SG, Santoro N, Soto-Greene M, Lasser N, Weiss G. Ethnic differences in insulin sensitivity and β -cell function in premenopausal or early perimenopausal women without diabetes: the study of women’s health across the nation (swan). Diabetes Care 27 (2): 2004; 354–361. [ DOI ] [ PubMed ]
- 184. Haffner S.M., Saad M.F., Rewers M., Mykkänen L., Selby J., Howard G., Savage P.J., Hamman R.F., Wegenknecht L.E., Bergman R.N. Increased insulin resistance and insulin secretion in nondiabetic african-americans and hispanics compared with non-hispanic whites: the insulin resistance atherosclerosis study. Diabetes. 1996;45(6):742–748. doi: 10.2337/diab.45.6.742. [ DOI ] [ PubMed ] [ Google Scholar ]
- 185. Rexrode K.M., Lee I.-M., Cook N.R., Hennekens C.H., Buring J.E. Baseline characteristics of participants in the women’s health study. J Women’s Health Gender-based Med. 2000;9(1):19–27. doi: 10.1089/152460900318911. [ DOI ] [ PubMed ] [ Google Scholar ]
- 186. Home. URL: https://www.cardia.dopm.uab.edu/ [Accessed on 03/03/2019].
- 187. Mahmood S.S., Levy D., Vasan R.S., Wang T.J. The framingham heart study and the epidemiology of cardiovascular disease: a historical perspective. The Lancet. 2014;383(9921):999–1008. doi: 10.1016/S0140-6736(13)61752-3. URL:http://www.sciencedirect.com/science/article/pii/S0140673613617523. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 188. Stahl C.H., Novak M., Lappas G., Wilhelmsen L., Björck L., Hansson P.-O., Rosengren A. High-normal blood pressure and long-term risk of type 2 diabetes: 35-year prospective population based cohort study of men. BMC Cardiovasc Disorders. 2012;12(1):89. doi: 10.1186/1471-2261-12-89. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 189. Wilhelmsen L., Berglund G., Elmfeldt D., Tibblin G., Wedel H., Pennert K., Vedin A., Wilhelmsson C., Werkö L. The multifactor primary prevention trial in göteborg, Sweden. Eur Heart J. 1986;7(4):279–288. doi: 10.1093/oxfordjournals.eurheartj.a062065. [ DOI ] [ PubMed ] [ Google Scholar ]
- 190. Kim B., Park J., Ahn Y., Kimm K., Shin C. Geographical difference in the prevalence of isolated systolic hypertension in middle-aged men and women in korea: the korean health and genome study. J Human Hypertension. 2005;19(11):877. doi: 10.1038/sj.jhh.1001904. [ DOI ] [ PubMed ] [ Google Scholar ]
- 191. C. for Disease Control, Prevention, et al. Behavioral risk factor surveillance system survey data. http://apps.nccd.cdc.gov/brfss/list.asp?cat=OH&yr-2008&qkey=6610&state=All.
- 192. Yoon P.W., Scheuner M.T., Peterson-Oehlke K.L., Gwinn M., Faucett A., Khoury M.J. Can family history be used as a tool for public health and preventive medicine? Gen Med. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 193. Tsenkova V.K., Karlamangla A.S., Ryff C.D. Parental history of diabetes, positive affect, and diabetes risk in adults: findings from midus. Ann Behav Med. 2016;50(6):836–843. doi: 10.1007/s12160-016-9810-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 194. Burchfiel C.M., Curb J.D., Rodriguez B.L., Yano K., Hwang L.-J., Fong K.-O., Marcus E.B. Incidence and predictors of diabetes in japanese-american men the honolulu heart program. Ann Epidemiol. 1995;5(1):33–43. doi: 10.1016/1047-2797(94)00038-u. [ DOI ] [ PubMed ] [ Google Scholar ]
- 195. Mitchell B.D., Valdez R., Hazuda H.P., Haffner S.M., Monterrosa A., Stern M.P. Differences in the prevalence of diabetes and impaired glucose tolerance according to maternal or paternal history of diabetes. Diabetes Care. 1993;16(9):1262–1267. doi: 10.2337/diacare.16.9.1262. [ DOI ] [ PubMed ] [ Google Scholar ]
- 196. Rodríguez-Moran M., Guerrero-Romero F., Aradillas-García C., Violante R., Simental-Mendia L.E., Monreal-Escalante E., De La Cruz Mendoza E. Obesity and family history of diabetes as risk factors of impaired fasting glucose: implications for the early detection of prediabetes. Pediatr Diabetes. 2010;11(5):331–336. doi: 10.1111/j.1399-5448.2009.00590.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 197. Valdez R., Yoon P.W., Liu T., Khoury M.J. Family history and prevalence of diabetes in the us population: the 6-year results from the national health and nutrition examination survey (1999–2004) Diabetes Care. 2007;30(10):2517–2522. doi: 10.2337/dc07-0720. [ DOI ] [ PubMed ] [ Google Scholar ]
- 198. Sargeant L., Wareham N., Khaw K. Family history of diabetes identifies a group at increased risk for the metabolic consequences of obesity and physical inactivity in epic-norfolk: a population-based study. Int J Obesity. 2000;24(10):1333. doi: 10.1038/sj.ijo.0801383. [ DOI ] [ PubMed ] [ Google Scholar ]
- 199. Suchindran S., Vana A.M., Shaffer R.A., Alcaraz J.E., McCarthy J.J. Racial differences in the interaction between family history and risk factors associated with diabetes in the national health and nutritional examination survey, 1999–2004. Genet Med. 2009;11(7):542. doi: 10.1097/GIM.0b013e3181a70917. [ DOI ] [ PubMed ] [ Google Scholar ]
- 200. Shaten B.J., Smith G.D., Kuller L.H., Neaton J.D. Risk factors for the development of type ii diabetes among men enrolled in the usual care group of the multiple risk factor intervention trial. Diabetes Care. 1993;16(10):1331–1339. doi: 10.2337/diacare.16.10.1331. [ DOI ] [ PubMed ] [ Google Scholar ]
- 201. Bjørnholt J.V., Erikssen G., Liestøl K., Jervell J., Thaulow E., Erikssen J. Type 2 diabetes and maternal family history: an impact beyond slow glucose removal rate and fasting hyperglycemia in low-risk individuals? results from 22.5 years of follow-up of healthy nondiabetic men. Diabetes Care. 2000;23(9):1255–1259. doi: 10.2337/diacare.23.9.1255. [ DOI ] [ PubMed ] [ Google Scholar ]
- 202. Meigs J.B., Cupples L.A., Wilson P.W. Parental transmission of type 2 diabetes: the framingham offspring study. Diabetes. 2000;49(12):2201–2207. doi: 10.2337/diabetes.49.12.2201. [ DOI ] [ PubMed ] [ Google Scholar ]
- 203. Thorand B., Liese A.D., Metzger M.-H., Reitmeir P., Schneider A., Löwel H. Can inaccuracy of reported parental history of diabetes explain the maternal transmission hypothesis for diabetes? Int J Epidemiol. 2001;30(5):1084–1089. doi: 10.1093/ije/30.5.1084. [ DOI ] [ PubMed ] [ Google Scholar ]
- 204. Knowler W.C., Pettitt D.J., Savage P.J., Bennett P.H. Diabetes incidence in pima Indians: contributions of obesity and parental diabetes. Am J Epidemiol. 1981;113(2):144–156. doi: 10.1093/oxfordjournals.aje.a113079. [ DOI ] [ PubMed ] [ Google Scholar ]
- 205. Lin R.S., Lee W.C., Lee Y.-T., Chou P., FU C.-C. Maternal role in type 2 diabetes mellitus: indirect evidence for a mitochondrial inheritance. Int J Epidemiol. 1994;23(5):886–890. doi: 10.1093/ije/23.5.886. [ DOI ] [ PubMed ] [ Google Scholar ]
- 206. Ishikawa-Takata K., Ohta T., Moritaki K., Gotou T., Inoue S. Obesity, weight change and risks for hypertension, diabetes and hypercholesterolemia in japanese men. Eur J Clin Nutr. 2002;56(7):601–607. doi: 10.1038/sj.ejcn.1601364. [ DOI ] [ PubMed ] [ Google Scholar ]
- 207. Collaboration A.P.C.S. Body mass index and risk of diabetes mellitus in the asia-pacific region. Asia Pacific. 2006;15(2):127–133. [ PubMed ] [ Google Scholar ]
- 208. Ohnishi H., Saitoh S., Takagi S., Katoh N., Chiba Y., Akasaka H., Nakamura Y., Shimamoto K. Incidence of type 2 diabetes in individuals with central obesity in a rural japanese population: the tanno and sobetsu study. Diabetes Care. 2006;29(5):1128–1129. doi: 10.2337/diacare.2951128. [ DOI ] [ PubMed ] [ Google Scholar ]
- 209. Hadaegh F., Zabetian A., Harati H., Azizi F. The prospective association of general and central obesity variables with incident type 2 diabetes in adults, tehran lipid and glucose study. Diabetes Res Clin Pract. 2007;76(3):449–454. doi: 10.1016/j.diabres.2006.09.030. [ DOI ] [ PubMed ] [ Google Scholar ]
- 210. He Y.-H., Jiang G.-X., Yang Y., Huang H.-E., Li R., Li X.-Y., Ning G., Cheng Q. Obesity and its associations with hypertension and type 2 diabetes among chinese adults age 40 years and over. Nutrition. 2009;25(11–12):1143–1149. doi: 10.1016/j.nut.2009.04.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 211. Bermudez O.I., Tucker K.L. Total and central obesity among elderly hispanics and the association with type 2 diabetes. Obesity Res. 2001;9(8):443–451. doi: 10.1038/oby.2001.58. [ DOI ] [ PubMed ] [ Google Scholar ]
- 212. Midus – midlife in the united states, a national longitudinal study of health and well-being. URL: http://midus.wisc.edu/ [Accessed on 03/04/2019].
- 213. Krishnan S., Rosenberg L., Djoussé L., Cupples L.A., Palmer J.R. Overall and central obesity and risk of type 2 diabetes in us black women. Obesity. 2007;15(7):1860–1866. doi: 10.1038/oby.2007.220. [ DOI ] [ PubMed ] [ Google Scholar ]
- 214. Flegal K.M., Carroll M.D., Ogden C.L., Johnson C.L. Prevalence and trends in obesity among us adults, 1999–2000. Jama. 2002;288(14):1723–1727. doi: 10.1001/jama.288.14.1723. [ DOI ] [ PubMed ] [ Google Scholar ]
- 215. Goryakin Y, Rocco L, Suhrcke M. The contribution of urbanization to non-communicable diseases: Evidence from 173 countries from 1980 to 2008. Econom Human Biol 26: 2017; 151–163. [ DOI ] [ PubMed ]
- 216. Hu F.B. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249–1257. doi: 10.2337/dc11-0442. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 217. Association A.D. Standards of medical care in diabetes: 2012. Diabetes Care. 2012;35(1):S11–S63. doi: 10.2337/dc12-s011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (864.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
Sep 13, 2023 · St. Petersburg, Fla. – September 12, 2023 – Scientists at Johns Hopkins All Children’s Hospital, along with an international team of researchers, are shedding new light on the causes of Type 2 diabetes. The new research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could ...
Nov 29, 2024 · Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency ...
This research will provide insights into the role of the brain in the control of blood sugar levels and has potential to facilitate the development of novel approaches to diabetes treatment.” The problem: Type 2 diabetes (T2D) is among the most pressing and costly medical challenges confronting modern society. Even with currently available ...
The purpose of this study is to evaluate the impact of a digital storytelling intervention derived through a community-based participatory research (CBPR) approach on type 2 diabetes mellitus (T2D) outcomes among Hispanic adults with poorly controlled type 2 diabetes mellitus (T2D) in primary care settings through a randomized clinical trial.
Amelioration of Both Central and Peripheral Neuropathy in Mouse Models of Type 1 and Type 2 Diabetes by the Neurogenic Molecule NSI-189. Diabetes, 68(11), 2143–2154. Read more. ADA-funded researcher studying link between ageing and type 2 diabetes. One of the most important risk factors for developing type 2 diabetes is age.
Type 2 Diabetes is thought to prevail in an individual from an interaction between several lifestyle, medical condition, hereditary, psychosocial and demographic risk factors such as high-level serum uric acid, sleep quality/quantity, smoking, depression, cardiovascular disease, dyslipidemia, hypertension, aging, ethnicity, family history of ...