An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Rheumatoid vasculitis: early presentation of rheumatoid arthritis
Yasir abdulqader, muhsen al-ani, konstantinos parperis.
- Author information
- Article notes
- Copyright and License information
Correspondence to Dr Yasir Abdulqader, [email protected]
Series information
Case Report
Accepted 2016 Oct 23; Collection date 2016.
Rheumatoid vasculitis is a rare and late complication of rheumatoid arthritis and may affect small-to-medium-sized vessels. Here, we report a case of a 49-year-old man who presented with amaurosis fugax in the left eye, symmetric polyarthritis, Raynaud's symptoms and paraesthesia in both lower extremities. The patient subsequently experienced right foot drop, nail fold infracts and gangrene of his right second toe. He was found to have a high titre of rheumatoid factor and treatment with rituximab and high dose of corticosteroids led to significant improvement of his symptoms. This is rare case describing the early onset of rheumatoid vasculitis in a patient with rheumatoid arthritis.
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterised by chronic symmetric polyarthritis and by the presence of autoantibodies including rheumatoid factor (RF) and anticyclic citrullinated peptide (anti-CCP) antibodies. Rheumatoid vasculitis (RV) is an unusual manifestation of chronic, deforming RA and may affect multiple systems. 1 2 The skin is commonly affected but other organs can be involved. RV should be in the differential diagnosis of patients presenting with multiple organ dysfunction and high titre of RF. We report a case of a patient with recently diagnosed RA which was complicated with systemic RV. Most often it occurs in patients with long-standing disease but in our case it was an initial presentation of the disease.
Case presentation
A 49-year-old African-American man, a chronic smoker, with no significant medical history presented with 3-day history of painless vision loss in the left eye, which resolved spontaneously, accompanied with a 2-month history of persistent bilateral hand, knee and elbow pain. He also experienced numbness of his lower extremities and intermittent bluish discolouration of the fingers and toes when exposed to cold. On examination, he was found to have synovitis bilaterally in the proximal interphalangeal and the metacarpophalangeal joints. Eye examination showed no evidence of retinal vein or artery occlusion.
Investigations
The following laboratory values were significant for RF of 4350 IU/mL, positive antinuclear antibodies with titre of 1:160, erythrocyte sedimentation rate of 80 mm/hour, C reactive protein of 9.47 mg/L, slightly elevated C3 and C4, 185 and 54 mg/dL, respectively. Anti-CCP antibodies, antineutrophil cytoplasmic antibodies (ANCAs), HIV antibodies, acute hepatitis panel, scleroderma-70 antibody, double-stranded DNA antibody, anti-SSA/anti-SSB autoantibodies, anti-Smith, antiphospholipid antibodies and cryoglobulins were all negative. X-rays of bilateral hands and feet showed no erosive changes or joint space narrowing.
Differential diagnosis
The differential diagnoses included vasculitis, infective endocarditis, peripheral artery disease, cryoglobulinaemia and thromboembolic disease.
Cerebrovascular accident was excluded by MRI and MR angiogram (MRA) of the brain and bilateral carotids ultrasound scan were within normal limits. Echocardiogram did not show any evidence of valve vegetation, intracardiac masses or thrombi. Blood cultures were obtained and were negative. The ankle brachial index test was within normal limit. CT angiogram of the abdomen was performed to rule out polyarteritis nodosa and there were no radiographical findings of intra-abdominal vascular aneurysms or stenosis.
The patient was started on prednisone 60 mg daily with taper instructions and methotrexate 15 mg weekly with folic acid 1 mg daily. Two months later, the patient stopped taking his medications and he developed worsening purple discolouration of his hands and feet, worse when exposed to cold, associated with nail fold and digits infractions in his hands and feet. He also presented with a necrotic ulcerative lesion on his right second toe and difficulty ambulating due to right foot drop (figure 1 A, B).

(A and B) A necrotic ulcerative lesion on the right second toe.
He was admitted with the working diagnosis of RV based on the presence of ulcerative necrotic lesion of his toe, mononeuritis multiplex with foot drop, history of polyarthritis, unexplained vision loss and high titre of RF. His RF was rechecked and found to be 7000 IU/mL. He received pulse dose of corticosteroids (1000 mg methylprednisolone for 3 days and then prednisone 60 mg daily while in the hospital), and total of two doses of Rituximab 1000 mg 2 weeks apart. For his ischaemic lesions and Raynaud's, the patient was treated with amlodipine 10 mg daily, aspirin 325 mg daily and topical nitroglycerine. The patient showed improvement of his symptoms except the right second toe's ulcerative lesion which worsened and he underwent amputation. Two days after the procedure the patient was discharged on prednisone 60 mg daily with tapering 5 mg every 1 week and methotrexate 20 mg weekly.
Outcome and follow-up
In a follow-up visit 3 months later, the patient noted improvement of his skin lesions, right foot strength, paraesthesia, Raynaud's phenomenon and denied joint pain or swelling. Repeated inflammatory markers showed a C reactive protein of 6.68 mg/L and sedimentation rate of 31 mm/hour.
RV is an unusual complication of long-standing, severe RA. It is characterised by an inflammatory process affecting small-to-medium-sized vessels and may involve any organ of the body. The mean duration between the diagnosis of RA and the onset of vasculitis is 10–14 years and it is unusual to be presented within the first 5 years of RA diagnosis though it has been reported before. 1 2 The 30-year incidence of vasculitis in patients with RA was estimated to be 3.6%. 1 Over the past 15 years, with the widespread use of biological agents early in the treatment of RA, has led to a decline in the prevalence of RV. 3
The postulated pathogenic mechanism of RV is complex, involving the activation of the endothelial cells, with upregulated expression of HLA-DQ, interleukin-1α and expansion of CD28 null T cells. 4 5 Several clinical studies suggest that RV may be caused by circulating immune complexes containing RF and autoantibodies such as antiendothelial cell antibodies, forming deposits in vessel walls and triggering an inflammatory reaction, which may lead to endothelial cell injury. 6 7
Risk factors for RV include long-standing RA, male, smoking, rheumatoid nodules and HLA class I and class II genotypes. 8 9 A genetic predisposition appears to be related to the development of RV in patients with RA. A meta-analysis that compiled 14 studies encompassing more than 1500 patients with RA revealed a strong relationship between RV and three specific genotypes of the HLA-DRB1. 10
The two most common organs to be involved are the skin and the peripheral nerves in more than 80% of patients. 11 Other system involvement includes heart, bowel and kidney which are much less common but can lead to significant morbidity and mortality, including myocardial infarction, bowel ischaemia and renal failure. 12 13
Cutaneous manifestations of RV include palpable purpura, nodules, ulcers, nail fold infractions, digital necrosis, livedo reticularis and urticarial vasculitis.
Diagnostic criteria for systemic RV were proposed by Scott and Bacon as having one or more of the following in the presence of RA: (1) mononeuritis multiplex or peripheral neuropathy, (2) peripheral gangrene, (3) biopsy evidence of acute necrotising arteritis in addition to systemic illness (fever and weight loss), and (5) deep cutaneous ulcers or extra-articular disease (eg, pleurisy, pericarditis and scleritis) if associated with typical digital infarcts or biopsy evidence of vasculitis. 14 15
Laboratory tests may support, but do not confirm the diagnosis of RV. Some studies have shown an association between high titres of RF or anti-CCP antibodies and RV. 16 Low complement has been associated with RV in 20–57% of the patients based on different studies. 17 18
Management includes the use of corticosteroids, cyclophosphamide, traditional and biological disease-modifying antirheumatic drugs (DMARDs). 19 The emergence of rituximab during the past decade as a new treatment of ANCA-associated vasculitis and RA was followed by the use of rituximab in RV. It showed a remarkable effect in inducing and maintaining remission, plus decreasing the incidence of relapse. 20
The prognosis in RV depends in part on the severity of the damage to the organs involved. Infection and end-organ damage from active vasculitis are the main causes of death; 40% of patients die within 5 years of disease onset. 21
Learning points.
This case report highlights that rheumatoid vasculitis (RV) can be, even though rare, the initial presentation of rheumatoid arthritis (RA).
RV, although it is a late complication of chronic RA, can be presented at any time during the disease process.
Mononeuritis multiplex, manifested with foot drop in a patient with RA, could be a warning sign of RV.
RV should be in the differential diagnosis of patients presenting with multiple organ dysfunction and high titre of rheumatoid factor.
High-dose glucocorticoids and rituximab help in inducing remission in active RA, while methotrexate or azathioprine might help in maintenance therapy. Rituximab has been shown to be effective in treating RV. The effect of tumour necrosis factor inhibitors and other biological agents in treating severe, active RV still require further investigations.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
- 1. Makol A, Crowson CS, Wetter DA et al. Vasculitis associated with rheumatoid arthritis: a case–control study. Rheumatology (Oxford) 2014;53:890–9. 10.1093/rheumatology/ket475 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Turesson C, O'Fallon WM, Crowson CS et al. Extra-articular disease manifestations in rheumatoid arthritis: incidence trends and risk factors over 46 years. Ann Rheum Dis 2003; 62:722–7. 10.1136/ard.62.8.722 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Bartels C, Bell C, Rosenthal A et al. Decline in rheumatoid vasculitis prevalence among US veterans: a retrospective cross-sectional study. Arthritis Rheum 2009;60:2553–7. 10.1002/art.24775 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Martens PB, Goronzy JJ, Schaid D et al. Expansion of unusual CD4+ T cells in severe rheumatoid arthritis. Arthritis Rheum 1997;40:1106–14. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Michel JJ, Turesson C, Lemster B et al. CD56-expressing T cells that have features of senescence are expanded in rheumatoid arthritis. Arthritis Rheum 2007;56:43–57. 10.1002/art.22310 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Jans H, Halberg P, Lorenzen I. Circulating immune complexes in rheumatoid arthritis with extra-articular manifestations. Scand J Rheumatol 1983;12:215–18. 10.3109/03009748309098536 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Scott DGI, Bacon PA, Allen C et al. IgG rheumatoid factor, complement and immune complexes in rheumatoid synovitis and vasculitis: comparative and serial studies during cytotoxic therapy. Clin Exp Immunol 1981;43:54–63. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Turesson C, Schaid DJ, Weyand CM et al. Association of HLA-C3 and smoking with vasculitis in patients with rheumatoid arthritis. Arthritis Rheum 2006;54:2776–83. 10.1002/art.22057 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Struthers GR, Scott DL, Delamere JP et al. Smoking and rheumatoid vasculitis. Rheumatol Int 1981;1:145–6. 10.1007/BF00541260 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Gorman JD, David-Vaudey E, Pai M et al. Particular HLA-DRB1 shared epitope genotypes are strongly associated with rheumatoid vasculitis. Arthritis Rheum 2004;50:3476–84. 10.1002/art.20588 [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Puechal X, Said G, Hilliquin P et al. Peripheral neuropathy with necrotizing vasculitis in rheumatoid arthritis. A clinicopathologic and prognostic study of thirty-two patients. Arthritis Rheum 1995;38:1618–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Caballol Pons N, Montalà N, Valverde J et al. Isolated cerebral vasculitis associated with rheumatoid arthritis. Joint Bone Spine 2010;77:361–3. 10.1016/j.jbspin.2010.02.030 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Zolcinski M, Bazan-Socha S, Zwolinska G et al. Central nervous system involvement as a major manifestation of rheumatoid arthritis. Rheumatol Int 2008;28:281–3. 10.1007/s00296-007-0428-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Scott DG, Bacon PA. Intravenous cyclophosphamide plus methylprednisolone in treatment of systemic rheumatoid vasculitis. Am J Med 1984;76:377–84. 10.1016/0002-9343(84)90654-5 [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Scott DG, Bacon PA, Tribe CR. Systemic rheumatoid vasculitis: a clinical and laboratory study of 50 cases. Medicine (Baltimore) 1981;60:288 10.1097/00005792-198107000-00004 [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Laskari K, Ahmadi-Simab K, Lamken M et al. Are anti-cyclic citrullinated peptide autoantibodies seromarkers for rheumatoid vasculitis in a cohort of patients with systemic vasculitis? Ann Rheum Dis 2010;69:469–71. 10.1136/ard.2009.110411 [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Franco AE, Schur PH. Hypocomplementemia in rheumatoid arthritis. Arthritis Rheum 1971;14:231–8. 10.1002/art.1780140206 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Schneider HA, Yonker RA, Katz P et al. Rheumatoid vasculitis: experience with 13 patients and review of the literature. Semin Arthritis Rheum 1985;14:280–6. 10.1016/0049-0172(85)90047-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Turesson C, Matteson EL. Management of extraarticular disease manifestations in rheumatoid arthritis. Curr Opin Rheumatol 2004;16:206–11. 10.1097/00002281-200405000-00007 [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Puéchal X, Gottenberg JE, Berthelot JM et al. Rituximab therapy for systemic vasculitis associated with rheumatoid arthritis: results from the AutoImmunity and Rituximab Registry. Arthritis Care Res (Hoboken) 2012;64:331–9. 10.1002/acr.20689 [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Voskuyl AE, Zwinderman AH, Westedt ML et al. The mortality of rheumatoid vasculitis compared with rheumatoid arthritis. Arthritis Rheum 1996;39:266–71. 10.1002/art.1780390213 [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (307.3 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Atypical presentation of rheumatoid arthritis: a case of massive bilateral pleural effusions in a patient with Caplan syndrome
Philip c dittmar.
- Author information
- Article notes
- Copyright and License information
Correspondence to Dr Philip C Dittmar; [email protected]
Corresponding author.
Series information
Case report
Accepted 2019 Oct 10; Collection date 2019.
Rheumatoid arthritis (RA) is a common connective tissue disorder affecting the synovial joints. In patients with RA, involvement of the lungs occurs in 30%–40% of cases while pleural effusions occur in only 3%–5%. However, the majority of RA-associated pleural effusions are small, unilateral and asymptomatic. We present a case of massive bilateral pleural effusions in a patient with established rheumatoid pneumoconiosis (Caplan syndrome). Interestingly, the pleural effusion occurred following recent treatment for minimal change disease and atrial fibrillation.
Keywords: rheumatoid arthritis, respiratory medicine
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disorder that commonly affects synovial joints. In certain susceptible individuals, exposure to coal, silica and/or asbestos can also lead to rheumatoid pneumoconiosis (Caplan syndrome). 1 2 Although Caplan syndrome by itself generally does not require treatment, management is directed towards treating the extrapulmonary manifestations of RA.
In patients with RA, 30%–40% have associated lung disease, most commonly involving the interstitium, airways or pleura. 3 The prevalence of pleural involvement is 50%–70% in autopsy studies, but symptomatic RA-associated pleural effusions occur in only 3%–5% of patients. 4 5 While a few case reports have reported on pleural effusions in patients with pulmonary nodules, the majority of these pulmonary nodules are asymptomatic and are discovered incidentally during or after thoracentesis. 6–10 To our knowledge, this is the first case of a patient with well-established Caplan syndrome who developed massive bilateral pleural effusions >20 years after his initial diagnosis.
Case presentation
A 74-year-old man with a history of RA complicated by Caplan syndrome (biopsy-proven silico-anthracotic pulmonary nodules), new-onset atrial fibrillation of 2-week duration and minimal change disease recently treated with steroids was admitted for persistent chest pain and shortness of breath. He described the pain as burning, substernal, non-radiating and worse on deep inspiration but denied any fever, chills, orthopnea, paroxysmal nocturnal dyspnea or leg swelling. When lying down, the pain localised to his mid-lower back. Family history was negative for autoimmune diseases. He had no significant alcohol or smoking history. Interestingly, he had worked in shipyards during his military service and as a porter for >20 years thereafter.
While in the emergency department, he was afebrile, tachypneic, tachycardic and normotensive saturating 95% on 2 L nasal cannula. His cardiovascular exam revealed an irregularly irregular rhythm. Lung exam revealed diminished breath sounds in the left lung base. Extremities showed multiple RA nodules on extensor surfaces of his forearms. The remainder of his exam was unremarkable.
Investigations
Routine serum chemistries and complete blood count were largely within normal limits but an electrocardiogram revealed atrial fibrillation with rapid ventricular response. CT angiography was negative for pulmonary embolus and revealed a moderate-sized left pleural effusion, small right pleural effusion and multiple bilateral pulmonary nodules (consistent with his previous diagnosis of Caplan syndrome). He was started on apixaban and intravenous metoprolol with gradual improvement in his chest pain and control of his heart rate.
On hospital day 2, he still appeared dyspneic. Due to concern for infection, blood and urine cultures were drawn. His urine culture grew Klebsiella pneumoniae for which he was started on ceftriaxone for coverage of a urinary tract infection and potential pneumonia. Overnight on hospital day 3, he acutely worsened and developed a new oxygen requirement with oxygen desaturations of 85%–95% on 5 L nasal cannula and decreased left lower lung sounds and increased mid-lower back pain. Laboratory studies revealed an elevated sedimentation rate (70 mm/hour, ref: 0–22 mm/hour) and highly elevated C-reactive protein (295 mg/L, ref: <3 mg/L). Repeat CT scan of the chest revealed an increased left-sided pleural effusion, mediastinal shift towards the right, complete consolidation of the left lower lobe with partial consolidation of the left upper lobe and a small right pleural effusion with associated atelectasis ( figure 1A ). At this point, rheumatology was consulted for assistance with management.
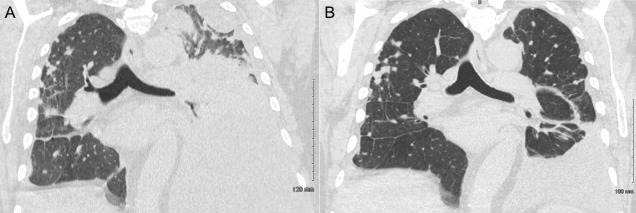
Thoracentesis and intravenous steroids led to a significant reduction in RA-associated pleural effusion burden. (A) Chest CT before treatment revealed a large, multiloculated left pleural effusion occupying the majority of the left hemithorax with mediastinal shift towards the right and a small right pleural effusion. (B) Chest CT after thoracentesis and three doses of intravenous methylprednisolone 125 mg administered once daily revealed a marked reduction in the size of the left pleural effusion with a persistent small right-sided pleural effusion. RA, rheumatoid arthritis.
On hospital day 5, thoracentesis removed 2 L of straw-coloured pleural fluid and a pigtail catheter was placed in the pleural space to drain residual fluid. Pleural fluid analysis revealed many polymorphonuclear cells without any organisms, 13.8 x 10 9 cells/L (97% neutrophils), glucose <1 mmol/L, protein 45 g/L, lactate dehydrogenase (LDH) 2514 IU/L, cholesterol 2.5 mmol/L, rheumatoid factor 96 IU/mL (ref: <16 IU/mL); serum levels revealed glucose 6.8 mmol/L, protein 55 g/L, LDH 182 IU/L, cholesterol 2.6 mmol/L ( table 1 ).
Analysis of RA-associated pleural fluid revealed an exudative effusion
*Normal reference ranges in parentheses.
LDH, lactate dehydrogenase; RA, rheumatoid arthritis.
Differential diagnosis
The first step in the evaluation of patients with a pleural effusion is to determine if the effusion is transudative or exudative. 11 In our case, the effusion was exudative by Light’s criteria. 12 Most exudative effusions in the USA are caused by pneumonia, cancer or pulmonary embolism. 11 Our patient had a negative CT angiography, which effectively ruled out pulmonary embolism. Moreover, our patient was afebrile, normotensive and had a normal leucocyte count, which lowered our suspicion for an infectious aetiology such as pneumonia. Since our suspicion for pneumonia and pulmonary embolism were lower on our differential, that left us considering cancer versus other rare aetiologies.
Given our patient’s extensive rheumatological history and work-related exposures from working in shipyards in the military, rheumatoid-associated pleural effusion and malignant pleural effusion were high on our differential. Typically, the pleural effusion seen in rheumatoid-associated pleural effusion has exudative features with a high rheumatoid factor titer, cholesterol (>1.7 mmol/L) and LDH (>700 IU/L) along with low glucose (<3.3 mmol/L) and pH levels (<7.2). 13 In our case, pleural fluid analysis revealed a high rheumatoid factor titer; cytology did not reveal any evidence of malignancy. These laboratory features taken together confirmed our diagnosis of rheumatoid-associated pleural effusion.
Thoracentesis of 2 L of pleural fluid was both diagnostic and therapeutic. In addition to thoracentesis, apixaban was withheld and the patient was treated with methylprednisolone 125 mg intravenous for 3 days (first dose started on hospital day 4).
Supplemental oxygen was removed on hospital day 6 and his oxygen-saturation remained >90% on room air for >24 hours. Bedside ultrasound on hospital day 7 revealed residual pleural effusions but he remained medically and haemodynamically stable.
On hospital day 8, final chest CT revealed a significant reduction in the left-sided pleural fluid effusion ( figure 1B ). He was later discharged the same day on prednisone 60 mg/day with a planned taper until his outpatient follow-up appointment with rheumatology.
Outcome and follow-up
At 6 months post-thoracentesis and methylprednisolone therapy, the patient has been doing well and has been living comfortably at his retirement home. He is being followed regularly as an outpatient by his rheumatologist who notes that his RA has been well controlled. There has been no evidence of recurrence of his pleural effusions.
Although RA-associated pleural effusions are found in 50%–70% of autopsy studies, effusions that cause symptoms are rare and occur in only 3%–5% of patients (eg, pleuritic chest pain and dyspnea). 4 14 Moreover, some studies have demonstrated that pleurisy and pleural effusions tend to occur as a late manifestation of RA, particularly in patients who have associated rheumatoid nodules, which interestingly, our patient had (Caplan syndrome). 15
A few case reports have been published on RA-associated pleural effusions describing the characteristics of the effusion, clinical manifestations of the disease and steroid-based therapies, but to our knowledge, this is the first report of RA-associated pleural effusion occurring in a patient with previously established Caplan syndrome. 13 16–18 Moreover, the pleural effusion developed in the setting of recent steroid withdrawal and atrial fibrillation.
Pleural effusion in the context of atrial fibrillation and beta-blocker administration is a well-established phenomenon. 19 However, in this case, the pleural effusion is clearly favourable of a rheumatoid aetiology. Thus, prompt thoracentesis and treatment with intravenous steroids is of the utmost importance while awaiting definitive long-term therapy.
Learning points.
Massive pleural effusions can occur in patients with rheumatoid pneumoconiosis (Caplan syndrome), even if they have been stable/asymptomatic for many years prior.
Recent withdrawal of steroids and/or atrial fibrillation in patients with rheumatoid arthritis (RA) may potentially trigger worsening of rheumatoid-associated pleural effusions.
Patients with suspected RA-associated pleural effusion should be evaluated via chest imaging and diagnostic/therapeutic thoracentesis followed by serum and pleural fluid analysis and cytology.
Analysis and cytology of RA-associated pleural effusions will reveal (1) an exudative effusion by Light’s criteria, (2) glucose <3.3 mmol/L, (3) elevated lactate dehydrogenase >700 U/L, (4) high rheumatoid factor titers and (5) inflammatory pleural fluid with a neutrophilic predominance.
Acute management with high-dose intravenous steroids and thoracentesis can lead to rapid symptomatic improvement; a gradual steroid-taper can be utilised while awaiting definitive long-term RA therapy with biologics.
Twitter: @PDittyMD
Contributors: YW conceived of the presented idea. YW and PCD contributed to the design, drafting and revision of the manuscript and final approval of the version to be published. YW and PCD agree to be accountable for the manuscript and to ensure that all questions regarding the accuracy or integrity of the manuscript are investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
- 1. Schreiber J, Koschel D, Kekow J, et al. . Rheumatoid pneumoconiosis (Caplan's syndrome). Eur J Intern Med 2010;21:168–72. 10.1016/j.ejim.2010.02.004 [ DOI ] [ PubMed ] [ Google Scholar ]
- 2. De Capitani EM, Schweller M, Silva CMda, et al. . Rheumatoid pneumoconiosis (Caplan's syndrome) with a classical presentation. J Bras Pneumol 2009;35:942–6. 10.1590/s1806-37132009000900017 [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Fischer A, du Bois R. Interstitial lung disease in connective tissue disorders. Lancet 2012;380:689–98. 10.1016/S0140-6736(12)61079-4 [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Shaw M, Collins BF, Ho LA, et al. . Rheumatoid arthritis-associated lung disease. Eur Respir Rev 2015;24:1–16. 10.1183/09059180.00008014 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Jurik AG, Davidsen D, Graudal H. Prevalence of pulmonary involvement in rheumatoid arthritis and its relationship to some characteristics of the patients. A radiological and clinical study. Scand J Rheumatol 1982;11:217–24. 10.3109/03009748209098194 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Emmungil H, Yıldız F, Gözükara MY, et al. . Rheumatoid pleural effusion with nodular pleuritis. A rare presentation of rheumatoid arthritis. Z Rheumatol 2015;74:72–4. 10.1007/s00393-014-1462-4 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Tserkezoglou A, Metakidis S, Papastamatiou-Tsimara H, et al. . Solitary rheumatoid nodule of the pleura and rheumatoid pleural effusion. Thorax 1978;33:769–72. 10.1136/thx.33.6.769 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Chabalko JJ. Acute rheumatoid pleurisy with effusion and demonstration of a rheumatoid nodule in the pleura. Del Med J 1984;56:649–51. [ PubMed ] [ Google Scholar ]
- 9. Kimura K, Toyama K, Yoshida M, et al. . [Rheumatoid nodule diagnosed by thoracoscopy using flexible fiberoptic bronchoscope]. Nihon Kokyuki Gakkai Zasshi 1998;36:994–7. [ PubMed ] [ Google Scholar ]
- 10. Jones JS. An account of pleural effusions, pulmonary nodules and cavities attributable to rheumatoid disease. Br J Dis Chest 1978;72:39–56. 10.1016/0007-0971(78)90006-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Porcel JM, Light RW. Diagnostic approach to pleural effusion in adults. Am Fam Physician 2006;73:1211–20. [ PubMed ] [ Google Scholar ]
- 12. Light RW, Macgregor MI, Luchsinger PC, et al. . Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med 1972;77:507–13. 10.7326/0003-4819-77-4-507 [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Balbir-Gurman A, Yigla M, Nahir AM, et al. . Rheumatoid pleural effusion. Semin Arthritis Rheum 2006;35:368–78. 10.1016/j.semarthrit.2006.03.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Alunno A, Gerli R, Giacomelli R, et al. . Clinical, epidemiological, and histopathological features of respiratory involvement in rheumatoid arthritis. Biomed Res Int 2017;2017:1–8. 10.1155/2017/7915340 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Bouros D, Pneumatikos I, Tzouvelekis A. Pleural involvement in systemic autoimmune disorders. Respiration 2008;75:361–71. 10.1159/000119051 [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Chou C-W, Chang S-C. Pleuritis as a presenting manifestation of rheumatoid arthritis: diagnostic clues in pleural fluid cytology. Am J Med Sci 2002;323:158–61. 10.1097/00000441-200203000-00008 [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Corcoran JP, Ahmad M, Mukherjee R, et al. . Pleuro-pulmonary complications of rheumatoid arthritis. Respir Care 2014;59:e55–9. 10.4187/respcare.02597 [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Stout J, Hayes D, Rojas-Moreno C, et al. . Rheumatoid pleural effusions and trapped lung: an uncommon complication of rheumatoid arthritis. Am J Hosp Med 2015;7. [ Google Scholar ]
- 19. Hooper C, Lee YCG, Maskell N, et al. . Investigation of a unilateral pleural effusion in adults: British thoracic Society pleural disease guideline 2010. Thorax 2010;65 Suppl 2:ii4–17. 10.1136/thx.2010.136978 [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (328.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
VIDEO
COMMENTS
The specificity of a positive test for anti-CCP antibodies for the diagnosis of rheumatoid arthritis is 95%; in combination with a positive test for rheumatoid factor, the specificity increases to ...
Presentation of Case. Dr. Christine M. Parsons ... Bouquillard E, Combe B. A report of 21 cases of rheumatoid arthritis following Chikungunya fever: a mean follow-up of two years.
From 2017 to 2021, there was a 74% increase in the overall number of cases of syphilis in the United States. 19 Syphilis can cause oligoarticular or polyarticular inflammatory arthritis, and the ...
Case Report on Rheumatoid Arthritis. ... The at ypical presentation of . rheumatoid arthritis in an elderly woman: a . ... Rheumatoid arthritis (RA) is an autoimmune disease, characterized by ...
Source Reference: Teyeb Z, et al "Case report: aortitis associated with rheumatoid arthritis: a challenging rheumatoid vasculitis presentation" F1000Res 2020; 9: 1370. Share on Facebook. Opens in ...
Rheumatoid meningitis (RM) is a rare central nervous system (CNS) manifestation of rheumatoid arthritis (RA) with a wide spectrum of symptoms. We present a review of the literature with a rare illustrative case of a 61-year-old man with a history of seropositive rheumatoid arthritis (RA) who presented headaches, stroke-like symptoms and seizures.
This case report focused on a similar scenario in an elderly woman initially thought to have osteoarthritis but was diagnosed later with rheumatoid arthritis which brought much relief to her current predicament. Keywords: Atypical, rheumatoid arthritis, DMARDs, quality of life. Introduction
By reporting this case, we hope to encourage medical professionals to concentrate on diagnosing old patients with unusual presentation of rheumatoid arthritis. "Rheumatoid arthritis (RA) is a systemic autoimmune disease primarily affecting synovial tissue and leading to joint destruction and disability". 1 Approximately 0.3-1% of the ...
This case report highlights that rheumatoid vasculitis (RV) can be, even though rare, the initial presentation of rheumatoid arthritis (RA). RV, although it is a late complication of chronic RA, can be presented at any time during the disease process.
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disorder that commonly affects synovial joints. In certain susceptible individuals, exposure to coal, ... Case presentation. A 74-year-old man with a history of RA complicated by Caplan syndrome (biopsy-proven silico-anthracotic pulmonary nodules), new-onset atrial fibrillation of 2 ...